The Carlat Psychiatry Blog
The Table is Here. The Voices are Not.
RFK Jr. cleared the CDC vaccine panel. The cost: clinical judgment.
Read More
You Can Be Neurodivergent. And Still Need Care.
When Neurodivergence Becomes a Rejection of Treatment, Patients Lose
Read More
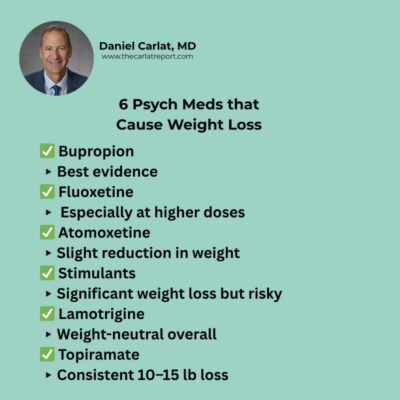
The Strange Side of Antidepressants
Fun facts from the upcoming Medication Fact Book, 8th Edition





_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)



