Home » Considerations When Prescribing Psychotropic Medications
Considerations When Prescribing Psychotropic Medications
May 1, 2018
From The Carlat Child Psychiatry Report
 Mark Chenven, MD
Private practice child and adolescent psychiatrist, San Diego, CA
Dr. Chenven has disclosed that he has no relevant financial or other interests in any commercial companies pertaining to this educational activity.
Mark Chenven, MD
Private practice child and adolescent psychiatrist, San Diego, CA
Dr. Chenven has disclosed that he has no relevant financial or other interests in any commercial companies pertaining to this educational activity.
CCPR: Thank you for joining us. To start things off, how do you approach using psychotropic medications for children and adolescents?
Dr. Chenven: Most parents do not want to start medications. I empathize with them, which then makes it possible to move together toward medications when indicated. I quote Dr. Oliver Wendell Holmes, Sr., who said, “If all the tools in man’s pharmacopeia were to be dumped into the sea, all the better for mankind and all the worse for the fishes.” While times have changed, the young, developing brain is still poorly understood; our DSM diagnostic template remains a work in progress; medications may be of limited benefit for many disorders; and access to high-quality and coordinated care is at best a rarity—even in the most advanced community systems of care.
CCPR: What else would you say about the challenges we face as clinicians while taking a psychopharmacology approach?
Dr. Chenven: There are pressures from all sides to use medications—it is often cheaper than psychotherapeutic and psychosocial interventions; the pharmaceutical industry has self-interests, and managed care leans that way too. Families in distress seek quick cures. Schools and social agencies must meet the needs of children and teens with multiple co-occurring challenges, and it’s good business for prescribers to prescribe early and often. That’s the environment in which we practice.
CCPR: It’s not all about the business of medicine, is it?
Dr. Chenven: Most prescription medications are safe, and when used judiciously, many are helpful. Medications can make a difference in the short term, and when meds work well, the benefits are life-changing—a child with ADHD can interact with family, teachers, and friends in normalized and normalizing ways so that the child’s psychosocial development gets back on track. An overly anxious teen calms and settles, sleeping soundly and managing responsibilities and social challenges. Life is better for everyone. So, yes, psychotropics have a valuable role to play. We just want to ensure that we’re not always simply reaching for the pill bottle.
CCPR: How important is it to consider lack of efficacy and side effects in prescribing decisions?
Dr. Chenven: There are times when medication treatments help only a bit, or only briefly. Often, presenting problems persist and evolve despite our best efforts. Additionally, well-intended treatments may exacerbate the patient’s clinical condition, with side effects or other unintended consequences. We often end up with Holmes’ dilemma—having an armamentarium whose benefit can be seen as uncertain or downright problematic.
CCPR: How can we manage this?
Dr. Chenven: The Hippocratic commitment to “do no harm” must be front and center. We need to judge whether a medication’s possible benefit outweighs its risks and whether the consequences of not prescribing may be worse. We need to know our patient well enough to decide whether to prescribe—in-depth knowledge of a child’s life at home, in the community, at school, and on the internet. Dr. George Engel’s biopsychosocial medical model for diagnosis, assessment, and treatment requires this level of clinical engagement, bridging the pharmacologic treatment, psychotherapeutic, and case management realms. Psychosocial interventions should never be underestimated. In a 1 + 1 = 3 paradigm, when medication is indicated, its appropriate use can be supplemented by well-formulated psychosocial interventions to optimize outcomes.
CCPR: I like that idea, 1 + 1 = 3. What about the family?
Dr. Chenven: Good prescribing practice is a partnership, as formulated in the Institute of Medicine’s “Crossing the Quality Chasm: A New Health System for the 21st Century” (see: http://bit.ly/2qcJrC6) and promulgated within systems of care guiding principles. Joint decision-making should be a central tenet in treatment. Working collaboratively in defining goals and in monitoring efficacy and side effects is simply good practice. Patient empowerment enhances compliance and improves decision-making.
CCPR: How do you monitor for side effects?
Dr. Chenven: Monitoring should be shared with patients and their parents, plus (with discretion) other caretakers such as teachers, therapists, primary care providers, program staff, etc. Educate even the youngest patients; let them know that we want to hear from them. Ask them, “Do you feel better?” relative to the treatment targets. Ask, “Is there anything about the medication that bothers or troubles you?” Our interest increases their propensity to self-evaluate and enhances our capacity to monitor their care. Use developmentally appropriate and culturally attuned language. With every new prescription, I review the common side effects and let the patient and parents know that it’s important for them to tell me about any concerns that arise, so we can discuss them collaboratively.
CCPR: How do you balance risks and benefits?
Dr. Chenven: All treatment should be assessed within a developmental context, with appreciation of short- and long-term costs and benefits. When a patient does not respond to interpersonal therapies, educational interventions, and the like, and if symptoms cause suffering or impinge upon developmental progression, considering medication should be part of the comprehensive treatment strategy.
CCPR: How does research help us to decide about medication for depression, or between stimulants and other meds for ADHD?
Dr. Chenven: Evidence-based practice brings in relevant research, clinical judgment and experience, and family culture/values as well as school and community context to make decisions. For depression in kids, placebo effects often match medication, yet on balance, research favors trying them (Locher C et al, JAMA Psychiatry 2017;74(10):1011–1020), especially when symptoms are severe, and when possible together with therapy. Decisions about ADHD medication consider side effects vs efficacy. Stimulants often have more of both, so while research supports trying them first, have a backup plan (Shier A et al, J Cent Nerv Syst Dis 2012;5:1–17).
CCPR: What about mood dysregulation?
Dr. Chenven: Irritability can seem nonspecific, and medications—antipsychotics and anticonvulsants—can be toxic. We need to look at the whole person. Is there poor sleep, a learning challenge, or a chronic ear infection at the root of it? In the spirit of the Research Diagnostic Criteria (RDoC) approach of NIMH in recent years, the concept of irritability is defined as a clinical entity associated with affective disorders (Vidal-Ribas P et al, J Am Acad Child Adolesc Psychiatry 2016;55(7):556–570). This may help guide us toward antidepressants before more problematic antipsychotics.
CCPR: What about parents who come in having given their child alprazolam or even cannabidiol oil? Or teens coming in and telling us that kratom is “perfectly safe”?
Dr. Chenven: For benzodiazepines, one study recently showed high rates of chronic use in children under 15 and called for regulating their use (O’Sullivan K et al, BMJ Open 2015;5(6):e007070). Educate parents about the limited efficacy, dangers of dependence, and impaired learning. CBD has been shown to help seizures and explored to treat schizophrenia, but marijuana more than doubles the rate of psychosis in young adults, with a dose-dependent increased risk in teens (Hall W and Degenhardt L, World Psychiatry 2008;7(2):68–71). CBD oil is interesting, but we do not have safety data nor regulation. Even recalcitrant teens often accept trials of more recognized medical approaches. Kratom is now getting attention, but there’s just no research to prove its safety or efficacy. At this point, I’d strongly advise against kratom.
CCPR: Thank you for your time, Dr. Chenven.
Child PsychiatryDr. Chenven: Most parents do not want to start medications. I empathize with them, which then makes it possible to move together toward medications when indicated. I quote Dr. Oliver Wendell Holmes, Sr., who said, “If all the tools in man’s pharmacopeia were to be dumped into the sea, all the better for mankind and all the worse for the fishes.” While times have changed, the young, developing brain is still poorly understood; our DSM diagnostic template remains a work in progress; medications may be of limited benefit for many disorders; and access to high-quality and coordinated care is at best a rarity—even in the most advanced community systems of care.
CCPR: What else would you say about the challenges we face as clinicians while taking a psychopharmacology approach?
Dr. Chenven: There are pressures from all sides to use medications—it is often cheaper than psychotherapeutic and psychosocial interventions; the pharmaceutical industry has self-interests, and managed care leans that way too. Families in distress seek quick cures. Schools and social agencies must meet the needs of children and teens with multiple co-occurring challenges, and it’s good business for prescribers to prescribe early and often. That’s the environment in which we practice.
CCPR: It’s not all about the business of medicine, is it?
Dr. Chenven: Most prescription medications are safe, and when used judiciously, many are helpful. Medications can make a difference in the short term, and when meds work well, the benefits are life-changing—a child with ADHD can interact with family, teachers, and friends in normalized and normalizing ways so that the child’s psychosocial development gets back on track. An overly anxious teen calms and settles, sleeping soundly and managing responsibilities and social challenges. Life is better for everyone. So, yes, psychotropics have a valuable role to play. We just want to ensure that we’re not always simply reaching for the pill bottle.
CCPR: How important is it to consider lack of efficacy and side effects in prescribing decisions?
Dr. Chenven: There are times when medication treatments help only a bit, or only briefly. Often, presenting problems persist and evolve despite our best efforts. Additionally, well-intended treatments may exacerbate the patient’s clinical condition, with side effects or other unintended consequences. We often end up with Holmes’ dilemma—having an armamentarium whose benefit can be seen as uncertain or downright problematic.
CCPR: How can we manage this?
Dr. Chenven: The Hippocratic commitment to “do no harm” must be front and center. We need to judge whether a medication’s possible benefit outweighs its risks and whether the consequences of not prescribing may be worse. We need to know our patient well enough to decide whether to prescribe—in-depth knowledge of a child’s life at home, in the community, at school, and on the internet. Dr. George Engel’s biopsychosocial medical model for diagnosis, assessment, and treatment requires this level of clinical engagement, bridging the pharmacologic treatment, psychotherapeutic, and case management realms. Psychosocial interventions should never be underestimated. In a 1 + 1 = 3 paradigm, when medication is indicated, its appropriate use can be supplemented by well-formulated psychosocial interventions to optimize outcomes.
CCPR: I like that idea, 1 + 1 = 3. What about the family?
Dr. Chenven: Good prescribing practice is a partnership, as formulated in the Institute of Medicine’s “Crossing the Quality Chasm: A New Health System for the 21st Century” (see: http://bit.ly/2qcJrC6) and promulgated within systems of care guiding principles. Joint decision-making should be a central tenet in treatment. Working collaboratively in defining goals and in monitoring efficacy and side effects is simply good practice. Patient empowerment enhances compliance and improves decision-making.
CCPR: How do you monitor for side effects?
Dr. Chenven: Monitoring should be shared with patients and their parents, plus (with discretion) other caretakers such as teachers, therapists, primary care providers, program staff, etc. Educate even the youngest patients; let them know that we want to hear from them. Ask them, “Do you feel better?” relative to the treatment targets. Ask, “Is there anything about the medication that bothers or troubles you?” Our interest increases their propensity to self-evaluate and enhances our capacity to monitor their care. Use developmentally appropriate and culturally attuned language. With every new prescription, I review the common side effects and let the patient and parents know that it’s important for them to tell me about any concerns that arise, so we can discuss them collaboratively.
CCPR: How do you balance risks and benefits?
Dr. Chenven: All treatment should be assessed within a developmental context, with appreciation of short- and long-term costs and benefits. When a patient does not respond to interpersonal therapies, educational interventions, and the like, and if symptoms cause suffering or impinge upon developmental progression, considering medication should be part of the comprehensive treatment strategy.
CCPR: How does research help us to decide about medication for depression, or between stimulants and other meds for ADHD?
Dr. Chenven: Evidence-based practice brings in relevant research, clinical judgment and experience, and family culture/values as well as school and community context to make decisions. For depression in kids, placebo effects often match medication, yet on balance, research favors trying them (Locher C et al, JAMA Psychiatry 2017;74(10):1011–1020), especially when symptoms are severe, and when possible together with therapy. Decisions about ADHD medication consider side effects vs efficacy. Stimulants often have more of both, so while research supports trying them first, have a backup plan (Shier A et al, J Cent Nerv Syst Dis 2012;5:1–17).
CCPR: What about mood dysregulation?
Dr. Chenven: Irritability can seem nonspecific, and medications—antipsychotics and anticonvulsants—can be toxic. We need to look at the whole person. Is there poor sleep, a learning challenge, or a chronic ear infection at the root of it? In the spirit of the Research Diagnostic Criteria (RDoC) approach of NIMH in recent years, the concept of irritability is defined as a clinical entity associated with affective disorders (Vidal-Ribas P et al, J Am Acad Child Adolesc Psychiatry 2016;55(7):556–570). This may help guide us toward antidepressants before more problematic antipsychotics.
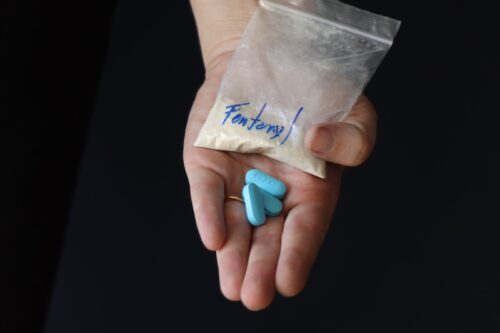
CCPR: What about parents who come in having given their child alprazolam or even cannabidiol oil? Or teens coming in and telling us that kratom is “perfectly safe”?
Dr. Chenven: For benzodiazepines, one study recently showed high rates of chronic use in children under 15 and called for regulating their use (O’Sullivan K et al, BMJ Open 2015;5(6):e007070). Educate parents about the limited efficacy, dangers of dependence, and impaired learning. CBD has been shown to help seizures and explored to treat schizophrenia, but marijuana more than doubles the rate of psychosis in young adults, with a dose-dependent increased risk in teens (Hall W and Degenhardt L, World Psychiatry 2008;7(2):68–71). CBD oil is interesting, but we do not have safety data nor regulation. Even recalcitrant teens often accept trials of more recognized medical approaches. Kratom is now getting attention, but there’s just no research to prove its safety or efficacy. At this point, I’d strongly advise against kratom.
CCPR: Thank you for your time, Dr. Chenven.
KEYWORDS child-psychiatry pharmacology-tips

Issue Date: May 1, 2018
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.



_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)