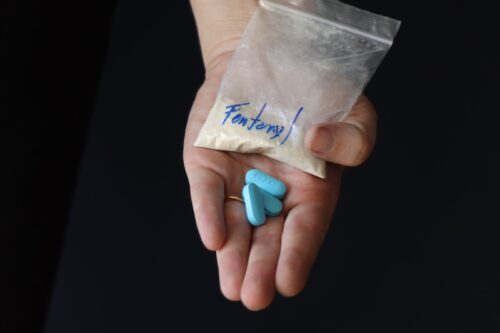
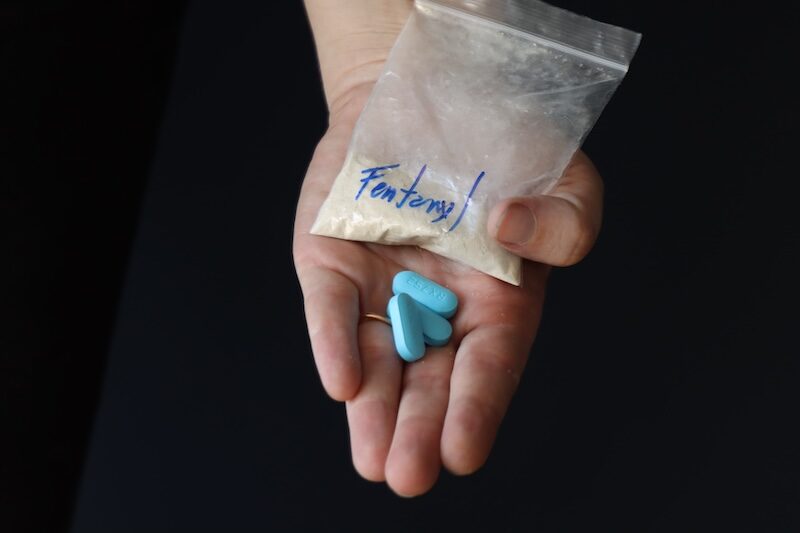
The Fentanyl overdose crisis is now one of the leading causes of death among adolescents, and it is happening in every corner of the country. Stay with us as we talk about the state of the crisis and the steps we can take to save lives.
Published On: 03/31/2025
Duration: 15 minutes, 41 seconds
Transcript:
JOSH FEDER: I am Dr. Josh Feder, the editor-in-chief of The Carlat Child Psychiatry Report and co-author of the Child Medication Factbook for Psychiatric Practice, second edition 2023, and the other book, Prescribing Psychotropics.
MARA GOVERMAN: And I'm Mara Goverman, a licensed clinical social worker in Southern California with a private practice and an avid reader of The Carlat Psychiatry Reports. Today, we are addressing an urgent public health issue affecting our youth—the fentanyl overdose crisis. The statistics are alarming in the US; there are over 100,000 drug overdose deaths each year, with opioids accounting for a large portion of these cases. Dr. Feder, could you provide an update on the current state of fentanyl overdoses among adolescents?
JOSH FEDER: Mara, it is one of the largest public health crises we have ever seen. Overdose deaths among teens have increased, get this more than 100% since the end of 2019. Right now, opioid overdoses are the third leading cause of death in adolescents age 14 to 18, right behind firearms and motor vehicle accidents. At the very beginning of my career, Mara, I thought I was gonna go into substance use. My career has been mostly trauma and autism, and I do a lot of that work. But the reason was because even back then, we are talking about the early nineties. We had problems then, and it is so much worse now. At that time, we were working with kids to try to help them role-play. How to say I do not want this stuff? It was in the age of just say no. And if you remember this, there was millions of dollars poured into that program, and it turned out it did not really work because it was a message without a methodology that was, could be shown to help kids to withstand the pressure from peers, but the role-playing that we did, it was called the Drugs and Kids Program, adopted by the American Bar Association of all places nationwide, and I think it went on to live for a while. I do not think it is around anymore, but the point that I am trying to make is that this problem has been with us for a very long time, and now it is amplified by fentanyl in particular.
MARA GOVERMAN: You mentioned fentanyl specifically; how exactly is this affecting our youths?
JOSH FEDER: Well, it is often accidental. They are popping a pill, thinking it is something like Xanax or Adderall that they bought off the street or from a friend. But it contains a deadly dose of fentanyl. A teen can take one pill, and it can end their life.
MARA GOVERMAN: So, in a way, it is not even about substance use disorder for many of these kids. Right? They are not necessarily seeking opioids.
JOSH FEDER: The largest group of teens overdosing are those who are not using opioids by choice. The second group is teens who have mental health struggles, anxiety, depression, ADHD, who might be more vulnerable to trying substances as a way to cope.
MARA GOVERMAN: I treated grandparents who lost their granddaughter, who took a pill at a party, who did not know what it was or where it came from, and tragically, she overdosed on fentanyl, then died.
JOSH FEDER: In the deaths in my clinical practice over the past, three or four decades early in my career, I did not see overdose deaths. Now, all of the losses that I have had in my practice, and you know, I am an old guy with a fairly big practice, have been overdose deaths, and all of them, I think, have been accidental in every single case. In the past, probably 15 years. So it is horrible.
MARA GOVERMAN: Yeah. In this age group, of being impulsive, and risk-taking, and being at a party, and not taking the time to think about what they're doing, adds so much to those statistics.
JOSH FEDER: That is right.
MARA GOVERMAN: And this does not just affect one group of teens, right? There are certain populations that are hit even harder than others.
JOSH FEDER: Yeah. Native American and Alaska Native adolescents have the highest rates of overdose death rates, about 80% higher than white teens, and Latinx youth are also more affected than their adult counterparts. In certain parts of the U.S., like Arizona, Colorado, and Washington State overdose death rates among teens are twice the national average.
MARA GOVERMAN: And where are they getting these pills from?
JOSH FEDER: Many still get them from family members or friends, even though opioid prescriptions are falling, there is still easy access to leftover medications at home. That is why it is so important for clinicians to have conversations with families about safe medications, storage, and disposal. Like you go to the dentist, and they automatically give you an opioid prescription to ease the pain, whatever. They do not even have to do that. I mean, they probably ought to be just recommending Motrin in almost every case or some other kind of NSAID, and yet people, maybe they use them, maybe they do not, they are lying around, and then people find them, and then they use them, and then they get addicted.
MARA GOVERMAN: Or overdose.
JOSH FEDER: Or overdose.
MARA GOVERMAN: What other strategies can clinicians use to prevent these overdoses?
JOSH FEDER: Well, harm reduction is the most important thing. We are seeing more widespread use of Narcan, which is great, and teens need to be trained on how to use it, just like adults, especially at schools, and things like that, they need to know how to use it. It has gotta be on hand, but also talking about the risks in schools, at home, and in healthcare settings, keeping that message vibrant and alive. It is not a one-time conversation. We need to talk about things like the danger of using drugs alone and recognizing overdose signs, and it is important for teens to learn how to use fentanyl test strips. You know, you are gonna take a pill. I do not want you to take the pill, but you should be testing it for fentanyl so that you do not die from using that pill that you bought from your buddy, and you thought was just fine.
MARA GOVERMAN: So, are you suggesting that parents have those hard and difficult conversation with their adolescents?
JOSH FEDER: Well, look in every appointment with any tween or teen, right? I am thinking about the big categories of things we should always be talking about. How is it going at home? How is it going at school? What is happening with activities and friends? What about substances have you been exposed to? Or What are you trying, and what is happening with dating, intimate relationships, stuff like that. We should be having those conversations every time we see them, modeling that, and when we talk to parents saying these are the things I talked to your kid about, and you need to be, kind of checking in with them as well, and I know they do not want to talk to you, but opening up that conversation is useful, and kids will often tell you things that you otherwise would not know. You certainly will not know if you do not ask.
MARA GOVERMAN: So, these are the tough topics that you have to talking about with your teens. But how do you do it in a way that resonates?
JOSH FEDER: Motivational interviewing is about building trust. Listening to a person, hearing their story, finding out what they want for their life, and then meeting them where they are and not just telling them what to do. Right? So, they wanna, I don't know, be good at sports, maybe play college sports. So, what will help you do that? What is gonna get in the way? Are you worried that the weed is gonna get in the way? Are you worried that the alcohol is gonna get in the way? Are you worried the fact that you are kind of finding pills from friends might get in the way? Same with opioid use obviously as well, then, typically when we are seeing those kids, their grades have already dropped, and we are doing other things maybe at a more intensive level of care to try to help them out, but in any case, you try to figure out what their goals are and then collaborate with them to try to help them to reach those goals, so they feel like they are making a decision to change, not being forced into it. We put out a motivational interviewing webinar, having to do more with weed at Carlat, probably a year ago, and I had like seven or so case examples, and one that comes to mind is a kid who I know just wanted to smoke weed and go to high school and be with his girlfriend, and that is kind of it. That is all he wanted to do, but I have stuck with him, and over the past year or so, we have worked toward a place where he is now out of high school and is reduced, and stopped alcohol and is reducing his weed because he is decided he actually likes the work he is doing and wants to improve on that and maybe even get an education surrounding it. So, it can happen. It is not easy, right? You gotta stick with people. But it can definitely work.
MARA GOVERMAN: You also talk about the educational component of drug use because the weed that they are selling today is so much stronger and might be full of chemicals, and I think this generation is focused on having something that is whole, that is organic, and that might also change their opinions about what they are smoking, and what they are thinking, and what they are ingesting.
MARA GOVERMAN: Also the neural anatomy of how it impacts a young brain.
JOSH FEDER: Right? I mean, it messes up your memory, and of course, it reduces your motivation, and then there is the medical stuff that happens too, right? The stomach aches, people coming into the ER for stomach problems.
MARA GOVERMAN: The lung issues.
JOSH FEDER: Oh, yes, of course. The pulmonary problems as well, people saying, Oh, it's weed, it is not gonna hurt my lungs. It does, and the vaping just as bad or worse.
MARA GOVERMAN: Okay, and with teens, these conversations matter, right? The adolescent brain is still developing, as we mentioned, and that can impact how they perceive risks.
JOSH FEDER: Yeah. Or not perceive them right?
MARA GOVERMAN: Or not perceive risks.
JOSH FEDER: Their prefrontal cortex is still developing, and they are not there planning ahead. I mean, that's so much of the problem. We can get people safely into their early twenties. A lot of times, you get more myelination, right? And people are making better choices. So, in the meantime, they're craving rewards. They're testing their limits, they're grappling with this high sense of justice and autonomy all at the same time, but parents can actually leverage some of that to encourage better decision-making. Kind of like what you're talking about in terms of like food safety justice, you know, what I mean? We shouldn't have these bad things in our food, and teaching them as well as we can, right, how to navigate peer pressure and support positive pro-social behaviors whenever we can, and that often means helping people engage in pro-social activities. Maybe it's taking care of other students who need mentoring or things like that, coaching other kids. Those kinds of responsible roles can be helpful.
MARA GOVERMAN: And it sounds like this takes a village, parents, clinicians, and the community all working together.
JOSH FEDER: And that is why it is important to have places with interdisciplinary teams to support these teens and their families. Peer recovery, coaching therapy, medication management. It is a holistic approach. It is not something that happens overnight like we talked about, but over time, with sustained support, we can make more progress. Mara and I were just talking a little bit earlier about some of the cases that don't work out and I think it is probably worth talking about these.
MARA GOVERMAN: Yes.
JOSH FEDER: I have a kid who has anxiety. He has been self-medicating with alcohol and weed for a long time, and we are not getting anywhere, and I worry about the long-term impact on this kid of where it is gonna go. There have been family members who have suffered consequences as adults because of their continued use, and we cannot always win these battles. But, you gotta kind of try. Part of what we talk about in this issue of The Carlat Child Psychiatry Report, that is for the Winter 2025, includes this piece on Fentanyl and the opioid crisis and also a piece on nicotine, maybe we will do a podcast on that.
MARA GOVERMAN: Yes.
JOSH FEDER: Because one of the things about these conditions is that you win some, and you lose some, and you are gonna lose some in this case. But that does not mean we stop trying. If we give up, we will lose a lot more. So that wraps up today's episode, not a very happy episode on the fentanyl overdose crisis affecting our youth. It is clear that this issue needs urgent attention from all of us: clinicians, families, and communities working together to make some impact. The goal is to reduce stigma and get teens the support they need to stay safe and to thrive.
MARA GOVERMAN: Absolutely, and if you are a parent educator or a healthcare provider, we encourage you to have those open, ongoing conversations with your teens, and of course, make sure you have Narcan on hand because one life saved can make all the difference.
JOSH FEDER: Dr. Aaron Quiggle’s interview in our January/February/March 2025 newsletter is the inspiration for this podcast, and it contains additional resources on how to prevent overdose and educate others. If you found this episode valuable, please share it with others who need to hear this message.
MARA GOVERMAN: Everything from Carlat Publishing is independently researched and produced. There is no funding from the pharmaceutical industry.
JOSH FEDER: Yes, the newsletters and books we produce depend entirely on reader support. There are no ads, and our authors do not receive industry funding. That helps us to bring you unbiased information that you can trust.
MARA GOVERMAN: Remember, we are all in this together. Stay informed, stay engaged, and let's continue the conversation.
JOSH FEDER: Thanks for tuning into The Carlat Child Psychiatry Podcast. Until next time, take care and stay safe.
__________
The Carlat CME Institute is accredited by the ACCME to provide continuing medical education for physicians. Carlat CME Institute maintains responsibility for this program and its content. Carlat CME Institute designates this enduring material educational activity for a maximum of one quarter (.25) AMA PRA Category 1 CreditsTM. Physicians or psychologists should claim credit commensurate only with the extent of their participation in the activity.

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)