Home » Helping Families Through the COVID-19 Pandemic
Helping Families Through the COVID-19 Pandemic
May 7, 2020
From The Carlat Child Psychiatry Report
Joshua Feder, MD.
Editor-in-Chief of CCPR. Practicing child psychiatrist, Solana Beach, CA. Adjunct Professor at Fielding Graduate University, CA.
Dr. Feder has disclosed that he has no relevant financial or other interests in any commercial companies pertaining to this educational activity.
The coronavirus has called on skills that few of us learned in our training. But you don’t need to be an epidemiologist or mental health expert to take some basic steps that will make this pandemic easier for your patients and families.
Telepsychiatry
Telehealth is becoming the norm, not the exception, and many private practices have shifted to phone and video mode. There are two ways to go about this. Some providers use a video app that is compliant with HIPAA, while others host visits through less secure software. In March 2020, the federal government announced a temporary relaxation of HIPAA restrictions, so that nearly any video software—including Skype, Google Hangouts, and FaceTime—can be used for telepsychiatry legally (www.tinyurl.com/s3v9h9t). There are some real advantages to telemedicine. You get to see your patients in their home environment, “play” with a child’s familiar toys, and coach parents without overshadowing them with your physical presence or the trappings of your office. Do stay mindful of the risks involved, including not knowing who else is listening on the other end.
Assessment and follow-up
If you usually check blood pressure, pulse, height, and weight and you can’t for the time being, think through the potential harms vs benefits and document your thinking in the medical record. Consider home blood pressure, pulse, height, and weight measurement. Often we forgo vital signs for stable patients who are away at college until they return on break. But growing children may need more careful follow-up, especially if there are medical problems or medication side effects. If unable to perform a necessary exam yourself, carefully weigh having patients seen somewhere else. Some things can be done on video, such as coaching patients through an Abnormal Involuntary Screening Exam.
Prescription refills
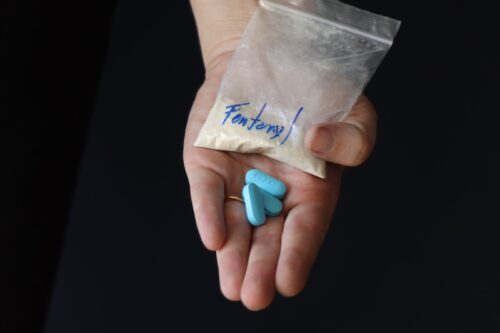
Medication shortages are a particular risk for our patients during a pandemic. When possible, multi-month prescriptions may be appropriate. Think about whether this is safe for patients who might misuse medications or are at risk for overdose, and document your thinking, including your advice to lock up supplies of medications.
Insurance challenges
Reimbursement for telehealth care is rapidly evolving. Many insurers are reimbursing phone visits during the outbreak. In March 2020, Medicare, and to a lesser extent Medicaid, vastly expanded coverage for telemedicine; most, if not all, commercial insurers are following suit (www.tinyurl.com/tjwsqsk). Check with your patient’s insurance company, or ask the patient to call them. If you are denied by an insurer, there are many ways to proceed. One is by going through your professional organizations—for example, the advocacy arm of the American Academy of Child and Adolescent Psychiatry (mgovaffairs@aacap.org). You can also call your congressional representative; find yours by using your residential ZIP code at www.house.gov/representatives/find-your-representative. Tell the staff that you’re a constituent—and that you need insurance reimbursement for online care. You can also call your state’s insurance commissioner’s office.
Online therapy resources
When families cannot obtain in-person therapy services, there are many online resources that can be helpful. While completion rates of online therapy programs are sometimes low (Fleming T et al, J Med Internet Res 2018;20(6):e199), we have a few favorites to share. www.profectum.org has a free online Parent Toolbox for families to support children and teens with autism and related challenges. The government of Australia has online CBT programs for anxiety and OCD (www.cci.health.wa.gov.au/Resources/Overview). And Albert Ellis’ book on rational emotive therapy, How to Control Your Anxiety Before It Controls You (Citadel, 2016), is free to listen to (www.tinyurl.com/y79qqu8j). There are also many phone apps to manage stress and promote mindfulness that are currently available for reduced cost. Some of my favorites include 10% Happier (www.tenpercent.com), Headspace (currently free for healthcare people; www.headspace.com), and Calm (www.calm.com).
The importance of schedules
Structured schedules are important for families quarantined at home. Going to bed at a reasonable hour, then getting up and getting dressed in daytime clothes at about the same time every day, is just good sleep hygiene. These steps alone may frame the days better. Here’s a great chapter that includes research on importance of routines:
www.ncbi.nlm.nih.gov/books/NBK402020. The day needs to emphasize hygiene and hydration. Time must be set aside for chores and cleaning both ourselves and our things—our new norm. Make time for schoolwork and for different kinds of activities, including movement (think dance, exercise, active games), creative pursuits (arts, crafts, music), and quiet time (reading, anyone?). Don’t forget about proper nutrition. Think about the life skills that kids can be learning while helping out. Finally, avoid too much news watching and be sure to address the news at the developmental level of the child you’re working with. Some days, structure and scheduling can go very smoothly, and on others productivity and expectations must give way to more generous compassion for ourselves and our families.
Value of play
It is hard to understate the value of symbolic play in helping children, teens, and also adults grapple with the emotional challenges of change, danger, and death (www.tinyurl.com/shq7yvg). Almost every enjoyable activity has meaning to it, so look at what attracts the child. Most sports, even indoor ones like Ping-Pong and billiards, have sublimated aggressive aspects and rely largely on skill; meanwhile, Candyland and other games of chance emphasize embracing things we cannot control. Some games, especially video games, combine both skill and chance, engaging us with the possibility of impacting our fate while knowing we cannot control everything. More complex play emerges with dolls, stuffed animals, writing or telling stories, and art. Parents can be active partners or an attentive audience, depending on the needs of the child.
Sleep is critical
Sleep deprivation makes it hard to manage stress. It also compromises the immune system, making people more susceptible to viral infections. Dim the lights and turn off electronic devices in the half hour before bed. Ideally, children and parents should sleep in a pitch-dark room, but if nighttime fears creep in, there are night lights free from the blue light that disrupts sleep. Check the offerings at www.lowbluelights.com or the Maxxima MLN-16 Amber LED Night Light (available at Amazon).
Supporting parents
This may be the most important thing you do. When parents do better, kids do better. Helping parents stay calm means helping them know that they are not alone in this. Telling them to “face the facts” is likely to create more stress. Telling them “I totally understand” is not true—as Tolstoy wrote in Anna Karenina, each unhappy family is unhappy in its own way. Instead, listen and note how hard it sounds, and validate their emotions. Set follow-up so families know you have them in mind. Providing support to parents will in turn help parents support their children.
Relationships with extended family and pets
The elderly are at high risk, and many are caring for children too. Grandparents can be a source of support and experience. Others are in assisted living or nursing homes and can’t receive visitors. Since not all seniors use videoconferencing, this gives kids a creative opportunity to make cards and write letters (properly sanitized, of course).
At this time, we do not think that pets carry or spread COVID-19. Patting and combing a willing pet can be calming. Teaching pets new skills is a great learning experience. For CDC information about pets, see www.tinyurl.com/vrg876v.
Advice for clinicians
It’s important to think about self-care as well. Most of us work too hard, and poor sleep and high stress further endangers us. Shut down the phone for 8 hours a night, fight the cravings for fat, salt, and sweets, and cultivate something that cools your head—what’s on your bucket list of safe activities? Be gentle with yourself. We need support too and can benefit from the same guidance we provide to others. Also, avoid oversharing your own difficulties with patients’ families.
CCPR Verdict: Many of these changes are good things to do anyway—it took the pandemic to put them in place.
Child PsychiatryTelepsychiatry
Telehealth is becoming the norm, not the exception, and many private practices have shifted to phone and video mode. There are two ways to go about this. Some providers use a video app that is compliant with HIPAA, while others host visits through less secure software. In March 2020, the federal government announced a temporary relaxation of HIPAA restrictions, so that nearly any video software—including Skype, Google Hangouts, and FaceTime—can be used for telepsychiatry legally (www.tinyurl.com/s3v9h9t). There are some real advantages to telemedicine. You get to see your patients in their home environment, “play” with a child’s familiar toys, and coach parents without overshadowing them with your physical presence or the trappings of your office. Do stay mindful of the risks involved, including not knowing who else is listening on the other end.
Assessment and follow-up
If you usually check blood pressure, pulse, height, and weight and you can’t for the time being, think through the potential harms vs benefits and document your thinking in the medical record. Consider home blood pressure, pulse, height, and weight measurement. Often we forgo vital signs for stable patients who are away at college until they return on break. But growing children may need more careful follow-up, especially if there are medical problems or medication side effects. If unable to perform a necessary exam yourself, carefully weigh having patients seen somewhere else. Some things can be done on video, such as coaching patients through an Abnormal Involuntary Screening Exam.
Prescription refills
Medication shortages are a particular risk for our patients during a pandemic. When possible, multi-month prescriptions may be appropriate. Think about whether this is safe for patients who might misuse medications or are at risk for overdose, and document your thinking, including your advice to lock up supplies of medications.
Insurance challenges
Reimbursement for telehealth care is rapidly evolving. Many insurers are reimbursing phone visits during the outbreak. In March 2020, Medicare, and to a lesser extent Medicaid, vastly expanded coverage for telemedicine; most, if not all, commercial insurers are following suit (www.tinyurl.com/tjwsqsk). Check with your patient’s insurance company, or ask the patient to call them. If you are denied by an insurer, there are many ways to proceed. One is by going through your professional organizations—for example, the advocacy arm of the American Academy of Child and Adolescent Psychiatry (mgovaffairs@aacap.org). You can also call your congressional representative; find yours by using your residential ZIP code at www.house.gov/representatives/find-your-representative. Tell the staff that you’re a constituent—and that you need insurance reimbursement for online care. You can also call your state’s insurance commissioner’s office.
Online therapy resources
When families cannot obtain in-person therapy services, there are many online resources that can be helpful. While completion rates of online therapy programs are sometimes low (Fleming T et al, J Med Internet Res 2018;20(6):e199), we have a few favorites to share. www.profectum.org has a free online Parent Toolbox for families to support children and teens with autism and related challenges. The government of Australia has online CBT programs for anxiety and OCD (www.cci.health.wa.gov.au/Resources/Overview). And Albert Ellis’ book on rational emotive therapy, How to Control Your Anxiety Before It Controls You (Citadel, 2016), is free to listen to (www.tinyurl.com/y79qqu8j). There are also many phone apps to manage stress and promote mindfulness that are currently available for reduced cost. Some of my favorites include 10% Happier (www.tenpercent.com), Headspace (currently free for healthcare people; www.headspace.com), and Calm (www.calm.com).
The importance of schedules
Structured schedules are important for families quarantined at home. Going to bed at a reasonable hour, then getting up and getting dressed in daytime clothes at about the same time every day, is just good sleep hygiene. These steps alone may frame the days better. Here’s a great chapter that includes research on importance of routines:
www.ncbi.nlm.nih.gov/books/NBK402020. The day needs to emphasize hygiene and hydration. Time must be set aside for chores and cleaning both ourselves and our things—our new norm. Make time for schoolwork and for different kinds of activities, including movement (think dance, exercise, active games), creative pursuits (arts, crafts, music), and quiet time (reading, anyone?). Don’t forget about proper nutrition. Think about the life skills that kids can be learning while helping out. Finally, avoid too much news watching and be sure to address the news at the developmental level of the child you’re working with. Some days, structure and scheduling can go very smoothly, and on others productivity and expectations must give way to more generous compassion for ourselves and our families.
Value of play
It is hard to understate the value of symbolic play in helping children, teens, and also adults grapple with the emotional challenges of change, danger, and death (www.tinyurl.com/shq7yvg). Almost every enjoyable activity has meaning to it, so look at what attracts the child. Most sports, even indoor ones like Ping-Pong and billiards, have sublimated aggressive aspects and rely largely on skill; meanwhile, Candyland and other games of chance emphasize embracing things we cannot control. Some games, especially video games, combine both skill and chance, engaging us with the possibility of impacting our fate while knowing we cannot control everything. More complex play emerges with dolls, stuffed animals, writing or telling stories, and art. Parents can be active partners or an attentive audience, depending on the needs of the child.
Sleep is critical
Sleep deprivation makes it hard to manage stress. It also compromises the immune system, making people more susceptible to viral infections. Dim the lights and turn off electronic devices in the half hour before bed. Ideally, children and parents should sleep in a pitch-dark room, but if nighttime fears creep in, there are night lights free from the blue light that disrupts sleep. Check the offerings at www.lowbluelights.com or the Maxxima MLN-16 Amber LED Night Light (available at Amazon).
Supporting parents
This may be the most important thing you do. When parents do better, kids do better. Helping parents stay calm means helping them know that they are not alone in this. Telling them to “face the facts” is likely to create more stress. Telling them “I totally understand” is not true—as Tolstoy wrote in Anna Karenina, each unhappy family is unhappy in its own way. Instead, listen and note how hard it sounds, and validate their emotions. Set follow-up so families know you have them in mind. Providing support to parents will in turn help parents support their children.
Relationships with extended family and pets
The elderly are at high risk, and many are caring for children too. Grandparents can be a source of support and experience. Others are in assisted living or nursing homes and can’t receive visitors. Since not all seniors use videoconferencing, this gives kids a creative opportunity to make cards and write letters (properly sanitized, of course).
At this time, we do not think that pets carry or spread COVID-19. Patting and combing a willing pet can be calming. Teaching pets new skills is a great learning experience. For CDC information about pets, see www.tinyurl.com/vrg876v.
Advice for clinicians
It’s important to think about self-care as well. Most of us work too hard, and poor sleep and high stress further endangers us. Shut down the phone for 8 hours a night, fight the cravings for fat, salt, and sweets, and cultivate something that cools your head—what’s on your bucket list of safe activities? Be gentle with yourself. We need support too and can benefit from the same guidance we provide to others. Also, avoid oversharing your own difficulties with patients’ families.
CCPR Verdict: Many of these changes are good things to do anyway—it took the pandemic to put them in place.
Issue Date: May 7, 2020
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)