Home » Primer: Evidence-Based Psychosocial Interventions for Substance Use Disorders
Primer: Evidence-Based Psychosocial Interventions for Substance Use Disorders
October 2, 2019
From The Carlat Addiction Treatment Report
Evidence-based psychosocial interventions form a critical component of substance use disorder (SUD) treatment. However, clinicians may be less familiar with some of the newer modalities. This primer will help you make informed referrals and discuss options with your patients.
Drug counseling
Addiction counselors are the backbone of SUD treatment. They support patients during recovery and encourage abstinence. They help patients develop relapse prevention plans by identifying a patient’s triggers and promoting lifestyle changes. Counselors may refer their patients to 12-step programs, support groups, or more specific psychotherapies.
Medical management
Addiction-focused medical management is a structured psychosocial intervention provided by medical professionals. The therapy aims to:
Clinicians may offer commonsense suggestions, such as telling patients to avoid going to bars. They also manage medications and attend to side effects (The Management of Substance Use Disorders Work Group. VA/DoD Clinical Practice Guideline for the Management of Substance Use Disorders. Version 3.0. https://www.healthquality.va.gov/guidelines/mh/sud/).
Cognitive behavioral therapy (CBT)
CBT forms the cornerstone of almost all therapeutic methods used for SUDs. It helps patients understand the connections between their thoughts, feelings, and behaviors, especially related to drug and alcohol use. Patients learn to challenge their thinking and change their actions using functional analysis. This helps them identify external triggers for substance use, such as specific people, places, and things, and to identify internal triggers using HALT—Hungry, Angry, Lonely, and Tired. Patients develop strategies to keep slips from turning into relapses; a slip is a temporary, unplanned use of a substance, while a relapse happens when the pattern of use meets SUD criteria after a period of remission. Patients in CBT also build skills and role-play difficult scenarios. See CATR May/June 2019 for more on CBT for SUDs.
In terms of efficacy, a meta-analysis of studies involving 2,340 patients found a moderate effect size (d = 0.45). The largest treatment effect was noted for cannabis, followed by cocaine and opioids, with the smallest impact reserved for polysubstance use. Similar results were noted for alcohol and drugs. Treatment benefit was sustained over time (McHugh RK et al, Psychiatr Clin North Am 2010;33(3):511–525).
A disadvantage perceived by some patients is that CBT involves homework assignments and worksheets. Another barrier is that CBT does not contain a clear method for addressing challenges such as non-adherence and conflict.
Motivational interviewing (MI)/motivational enhancement therapy (MET)
MI/MET is based on the idea that lasting, personal change is driven by internal motivation rather than external pressure. Ambivalence to change is considered part of the process. The primary tools are to address ambivalence and develop discrepancies between patients’ present behaviors and their goals and values. For example, I’ll ask patients to tell me what their future will look like if they keep using and what it could look like if they stop using. A discrepancy arises if the future they want doesn’t match the future predicted by continued use. MET is a manualized version of MI. It has an added feedback component that informs patients how their use compares with the general population.
MI/MET is an effective therapy. A review of 39 meta-analyses found moderate quality of evidence that MI was effective for stopping or preventing binge drinking and reducing the quantity and frequency of drinking, smoking, and substance misuse (Frost H et al, PLoS One 2018;13(10):e0204890).
One disadvantage is that it’s not recommended to reintroduce ambivalence in patients who have already resolved their ambivalence and decided they want to stop using. Also, giving information and advice is part of MI/MET, but this is done with permission and with a focus on patient autonomy—clinicians shouldn’t refrain from informing patients about the consequences of continued use, such as increased risk of death from IV heroin use.
Behavioral couples therapy (BCT)
BCT is a short-term manualized therapy that lasts for 12–20 weekly couples’ sessions over 3–6 months. Couples analyze factors contributing to a patient’s SUD and collaborate to improve the situation. Partners learn communication and problem-solving skills, as well as find shared activities not involving substance use. Couples create a “sobriety contract.” In it, the patient contracts with the partner daily to not drink or use drugs for that day. The partner then voices support for the patient’s efforts to stay abstinent. Couples may attend 12-step programs and therapy together. Partners may monitor medication adherence.
Overall, BCT produces better outcomes than individual-based treatments for married or cohabiting individuals seeking help for alcohol or drug use disorders. It has a moderate effect size (d = 0.45) over individual treatments in reducing frequency of use in couples (Powers MB et al, Clin Psychol Rev 2008;28(6):952–962).
Unfortunately, most treatment programs do not provide BCT, and many clinicians are unfamiliar with the therapy, despite its results (Fletcher AM. Inside Rehab: The Surprising Truth About Addiction Treatment and How to Get Help That Works. New York, NY: Viking; 2013). See https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3215582/ for a short guide on incorporating BCT concepts into your practice.
Contingency management (CM)
Imagine a therapy that rewards patients for staying sober. It’s called CM, and it works. Rewards, which help to increase recovery-oriented behaviors, are dependent on objective evidence like negative toxicology screens, treatment adherence, or meeting treatment goals. The most common rewards are vouchers with monetary value that can be redeemed for goods and services, or vouchers for prize incentives to be won in drawings.
In terms of outcomes, CM consistently shows improved treatment results for numerous SUDs, including stimulant use disorders. It can be implemented together with any psychotherapy or pharmacotherapy. Compared to other psychosocial treatments, it has the largest effect size (d = 0.6), with moderate to high effect (Petry NM et al, Psychol Addict Behav 2017;31(8):897–906).
CM is not in widespread use due to economic concerns—who pays for the rewards?—and therapeutic issues. Some worry it undermines the message of motivation-based and 12-step programs. It’s also uncertain whether CM continues to prevent relapse long-term, once the rewards have stopped (Petry NM et al, Psychol Addict Behav 2017;31(8):897–906). Due to its expense, this approach is better suited for organizations rather than individual practitioners.
Community reinforcement approach (CRA)
CRA is a multifaceted program for tackling addiction. The overall goal is to assist patients in adopting a sober lifestyle that is more rewarding than one full of drugs and alcohol. Patients look at the factors triggering and reinforcing their substance use. A therapist then helps them reengage and reconnect with healthy outlets such as family, friends, work, and hobbies, with the idea that these will replace the substance use. Patients also receive job skills training, relationship counseling, and substance refusal training, while working on problem-solving and relapse prevention skills.
CRA’s efficacy for alcohol use disorder is supported via several meta-analyses and research reviews. It’s also useful in drug use disorders, including patients using cocaine and opioids (Meyers RJ et al, Alcohol Res Health 2011;33(4):380–388). The biggest problem with CRA used to be its inaccessibility in the US (Fletcher AM. Inside Rehab: The Surprising Truth About Addiction Treatment and How to Get Help That Works. New York, NY: Viking; 2013). However, CRA principles are now in widespread use and part of most treatment programs.
Twelve-step facilitation (TSF)
TSF is a manualized treatment in which therapists use the principles from 12-step recovery programs like Alcoholics Anonymous (AA) in weekly therapy sessions. Denial and loss of control are central concepts. The recovery process places a strong focus on the power of spirituality—belief in “a power greater than ourselves.” Treatment goals are total abstinence and regular attendance.
Project MATCH (Matching Alcohol Treatment to Client Heterogeneity) was a large study comparing TSF, MET, and CBT. It found that patients treated with TSF attended more 12-step meetings, had comparable reductions in drinking, and had higher levels of overall abstinence than the other two treatments (Donovan DM et al, Soc Work Public Health 2013;28(3–4):313–332). All Project MATCH treatment manuals (TSF, MET, and CBT) are available at https://pubs.niaaa.nih.gov/publications/ProjectMatch/matchIntro.htm for free.
Due to the widespread availability of AA, TSF’s concepts are well known and accepted by most patients. Twelve-step programs and meetings are also readily accessed. One drawback for some patients is the emphasis on a higher power and loss of control.
CATR Verdict: Effective psychosocial interventions form a critical component of SUD treatment (see table above). These interventions work best when combined with medications for SUDs and when comorbid psychiatric disorders are also addressed. Unfortunately, clinicians often lack training in many of them.
Table: Psychosocial Interventions for Substance Use Disorder Treatment
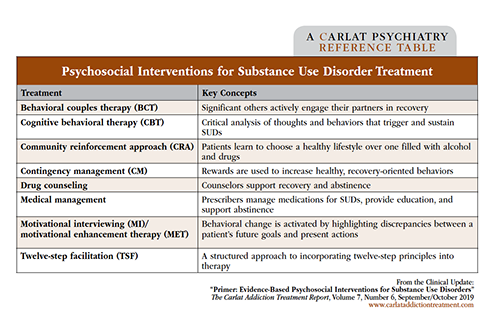
Click to view full-size PDF.
Addiction TreatmentBasic interventions
Drug counseling
Addiction counselors are the backbone of SUD treatment. They support patients during recovery and encourage abstinence. They help patients develop relapse prevention plans by identifying a patient’s triggers and promoting lifestyle changes. Counselors may refer their patients to 12-step programs, support groups, or more specific psychotherapies.
Medical management
Addiction-focused medical management is a structured psychosocial intervention provided by medical professionals. The therapy aims to:
- Enhance medication adherence and monitor for side effects
- Track substance use and its sequelae via self-report and laboratory tests
- Foster abstinence through education
- Provide referrals to community support groups
- Encourage lifestyle changes that sustain recovery
Clinicians may offer commonsense suggestions, such as telling patients to avoid going to bars. They also manage medications and attend to side effects (The Management of Substance Use Disorders Work Group. VA/DoD Clinical Practice Guideline for the Management of Substance Use Disorders. Version 3.0. https://www.healthquality.va.gov/guidelines/mh/sud/).
Common advanced interventions
Cognitive behavioral therapy (CBT)
CBT forms the cornerstone of almost all therapeutic methods used for SUDs. It helps patients understand the connections between their thoughts, feelings, and behaviors, especially related to drug and alcohol use. Patients learn to challenge their thinking and change their actions using functional analysis. This helps them identify external triggers for substance use, such as specific people, places, and things, and to identify internal triggers using HALT—Hungry, Angry, Lonely, and Tired. Patients develop strategies to keep slips from turning into relapses; a slip is a temporary, unplanned use of a substance, while a relapse happens when the pattern of use meets SUD criteria after a period of remission. Patients in CBT also build skills and role-play difficult scenarios. See CATR May/June 2019 for more on CBT for SUDs.
In terms of efficacy, a meta-analysis of studies involving 2,340 patients found a moderate effect size (d = 0.45). The largest treatment effect was noted for cannabis, followed by cocaine and opioids, with the smallest impact reserved for polysubstance use. Similar results were noted for alcohol and drugs. Treatment benefit was sustained over time (McHugh RK et al, Psychiatr Clin North Am 2010;33(3):511–525).
A disadvantage perceived by some patients is that CBT involves homework assignments and worksheets. Another barrier is that CBT does not contain a clear method for addressing challenges such as non-adherence and conflict.
Motivational interviewing (MI)/motivational enhancement therapy (MET)
MI/MET is based on the idea that lasting, personal change is driven by internal motivation rather than external pressure. Ambivalence to change is considered part of the process. The primary tools are to address ambivalence and develop discrepancies between patients’ present behaviors and their goals and values. For example, I’ll ask patients to tell me what their future will look like if they keep using and what it could look like if they stop using. A discrepancy arises if the future they want doesn’t match the future predicted by continued use. MET is a manualized version of MI. It has an added feedback component that informs patients how their use compares with the general population.
MI/MET is an effective therapy. A review of 39 meta-analyses found moderate quality of evidence that MI was effective for stopping or preventing binge drinking and reducing the quantity and frequency of drinking, smoking, and substance misuse (Frost H et al, PLoS One 2018;13(10):e0204890).
One disadvantage is that it’s not recommended to reintroduce ambivalence in patients who have already resolved their ambivalence and decided they want to stop using. Also, giving information and advice is part of MI/MET, but this is done with permission and with a focus on patient autonomy—clinicians shouldn’t refrain from informing patients about the consequences of continued use, such as increased risk of death from IV heroin use.
Other advanced interventions
Behavioral couples therapy (BCT)
BCT is a short-term manualized therapy that lasts for 12–20 weekly couples’ sessions over 3–6 months. Couples analyze factors contributing to a patient’s SUD and collaborate to improve the situation. Partners learn communication and problem-solving skills, as well as find shared activities not involving substance use. Couples create a “sobriety contract.” In it, the patient contracts with the partner daily to not drink or use drugs for that day. The partner then voices support for the patient’s efforts to stay abstinent. Couples may attend 12-step programs and therapy together. Partners may monitor medication adherence.
Overall, BCT produces better outcomes than individual-based treatments for married or cohabiting individuals seeking help for alcohol or drug use disorders. It has a moderate effect size (d = 0.45) over individual treatments in reducing frequency of use in couples (Powers MB et al, Clin Psychol Rev 2008;28(6):952–962).
Unfortunately, most treatment programs do not provide BCT, and many clinicians are unfamiliar with the therapy, despite its results (Fletcher AM. Inside Rehab: The Surprising Truth About Addiction Treatment and How to Get Help That Works. New York, NY: Viking; 2013). See https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3215582/ for a short guide on incorporating BCT concepts into your practice.
Contingency management (CM)
Imagine a therapy that rewards patients for staying sober. It’s called CM, and it works. Rewards, which help to increase recovery-oriented behaviors, are dependent on objective evidence like negative toxicology screens, treatment adherence, or meeting treatment goals. The most common rewards are vouchers with monetary value that can be redeemed for goods and services, or vouchers for prize incentives to be won in drawings.
In terms of outcomes, CM consistently shows improved treatment results for numerous SUDs, including stimulant use disorders. It can be implemented together with any psychotherapy or pharmacotherapy. Compared to other psychosocial treatments, it has the largest effect size (d = 0.6), with moderate to high effect (Petry NM et al, Psychol Addict Behav 2017;31(8):897–906).
CM is not in widespread use due to economic concerns—who pays for the rewards?—and therapeutic issues. Some worry it undermines the message of motivation-based and 12-step programs. It’s also uncertain whether CM continues to prevent relapse long-term, once the rewards have stopped (Petry NM et al, Psychol Addict Behav 2017;31(8):897–906). Due to its expense, this approach is better suited for organizations rather than individual practitioners.
Community reinforcement approach (CRA)
CRA is a multifaceted program for tackling addiction. The overall goal is to assist patients in adopting a sober lifestyle that is more rewarding than one full of drugs and alcohol. Patients look at the factors triggering and reinforcing their substance use. A therapist then helps them reengage and reconnect with healthy outlets such as family, friends, work, and hobbies, with the idea that these will replace the substance use. Patients also receive job skills training, relationship counseling, and substance refusal training, while working on problem-solving and relapse prevention skills.
CRA’s efficacy for alcohol use disorder is supported via several meta-analyses and research reviews. It’s also useful in drug use disorders, including patients using cocaine and opioids (Meyers RJ et al, Alcohol Res Health 2011;33(4):380–388). The biggest problem with CRA used to be its inaccessibility in the US (Fletcher AM. Inside Rehab: The Surprising Truth About Addiction Treatment and How to Get Help That Works. New York, NY: Viking; 2013). However, CRA principles are now in widespread use and part of most treatment programs.
Twelve-step facilitation (TSF)
TSF is a manualized treatment in which therapists use the principles from 12-step recovery programs like Alcoholics Anonymous (AA) in weekly therapy sessions. Denial and loss of control are central concepts. The recovery process places a strong focus on the power of spirituality—belief in “a power greater than ourselves.” Treatment goals are total abstinence and regular attendance.
Project MATCH (Matching Alcohol Treatment to Client Heterogeneity) was a large study comparing TSF, MET, and CBT. It found that patients treated with TSF attended more 12-step meetings, had comparable reductions in drinking, and had higher levels of overall abstinence than the other two treatments (Donovan DM et al, Soc Work Public Health 2013;28(3–4):313–332). All Project MATCH treatment manuals (TSF, MET, and CBT) are available at https://pubs.niaaa.nih.gov/publications/ProjectMatch/matchIntro.htm for free.
Due to the widespread availability of AA, TSF’s concepts are well known and accepted by most patients. Twelve-step programs and meetings are also readily accessed. One drawback for some patients is the emphasis on a higher power and loss of control.
CATR Verdict: Effective psychosocial interventions form a critical component of SUD treatment (see table above). These interventions work best when combined with medications for SUDs and when comorbid psychiatric disorders are also addressed. Unfortunately, clinicians often lack training in many of them.
Table: Psychosocial Interventions for Substance Use Disorder Treatment
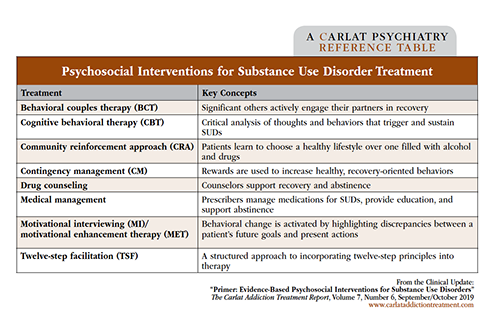
Click to view full-size PDF.
KEYWORDS addiction addiction-treatment cognitive_behavioral_therapy motivational-interviewing psychotherapy substance-use-disorder
Issue Date: October 2, 2019
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)



