Home » Diagnosing Depression in Children and Adolescents
Diagnosing Depression in Children and Adolescents
November 1, 2015
From The Carlat Child Psychiatry Report
Glen R. Elliott, PhD, MD
Today, the idea that adolescents and children, even young children, can have a major depressive disorder is widely accepted, but that was not always the case. Debates about the age at which “true” depression could manifest itself were widespread in child and adolescent psychiatry through the late 70s and into the early 80s (Pataki CS and Carlson GA, Harvard Rev Psychiatry 1995;3(3):140–151). With the introduction of DSM-III and its emphasis on objective signs and symptoms, researchers began to survey adolescents and latency-age children and found that a subgroup of these young patients indeed met criteria for major depression (Puig-Antich and Weston, Annual Rev Med 1983;34:231–245).
The prevalence of depression increases markedly with age (Manepalli et al, Current Psychiatry 2011; 10:20–24), with rates of about 0.3% of preschoolers, 0.5%–3% of prepubertal children, 0.5%–6.5% of teenagers, and 10%–17% of adults. While adult depression is twice as common in women as in men, that ratio is nearly 1:1 in prepubertal children. In the early teen years, roughly correlating with the onset of puberty, though not necessarily associated with it, depression rates rise much more rapidly in females, so that the adult ratio of 1:2 is achieved by early-to-mid teens. While we don’t understand why, the bottom line is that young boys are as likely to have depression as young girls, while teen girls are twice as likely to be depressed as teen boys.
Depression in adolescents
Aran was a 15-year-old Asian male whose parents came to the U.S. as young adults. He was academically gifted and committed to scholarly pursuits, which his parents strongly encouraged. He was somewhat of a loner but had friends; his parents perceived him as being happy and eager to please. They were conservative about him spending time on social media and the Internet but he never complained, did expected household chores, and was involved in school-sponsored clubs.
The summer before his 10th grade year, Aran began to spend more time in his room, complained of being tired and started sleeping 10–12 hours a night. He seemed to be always hungry, gaining 12 pounds in 10 weeks, and became apathetic about previous interests such as video games. When school started, he took much longer doing his homework and had particular trouble with an advanced math class, getting his first-ever B+. He and his parents were both upset, and hired a tutor. However, when Aran took the final, he was convinced he failed it. That evening, he would not talk to his parents, did not eat supper, and went to his room. Worried, they entered his room, where they found him holding a sharp knife that he had taken from the kitchen. Aran began crying and tried to stab himself. His parents were able to wrest the knife from him and took him to the nearest emergency room, where he was assessed and hospitalized for suicidality.
One might assume that adolescents, being almost adults, would be most apt to present with adult-like signs and symptoms of depression. In fact, they are more likely to have atypical depressive symptoms such as increased appetite with weight gain and increased need for sleep (Pataki CS and Carlson GA, Harvard Rev Psychiatry 1995;3(3):140–151). In addition, their mood is less persistent and more reactive to environmental setting than is true for depressed adults. With friends and at school, they may seem happy and untroubled, only to appear deeply depressed when they are alone or at home, which can be particularly baffling—and frustrating—for parents.
When evaluating adolescents for depression, I usually begin by meeting briefly with the whole family, and then with the patient alone. Adolescents are often angry about having been forced to come see me but generally calm once parents leave. I start by exploring neutral or positive aspects of their life such as interests, what they like most about school, and favorite shows or hobbies. I then ask why they think their parents brought them to see me. I ask specifically about mood, using a variety of terms such as “down,” “irritable,” “sad,” “upset,” and “moody” and sticking to whatever term the adolescent endorses. I also ask about a series of symptoms and experiences common in adolescent depression (See the “Tips for Diagnosing Depression” table on page 3). Equally important are questions about how the teen feels about the possibility of taking a medication to help with depression and discussing any concerns.
As with Aran’s scenario, depressed adolescents are at high risk for suicidal ideation. Some estimates suggest that as many as 60% of all adolescents think about killing themselves or that their family would be better off without them at least once during adolescence, though obviously for the vast majority it is idle speculation (VanderStoep A et al, Suicide Life Threat Behav 2009;39(6):599–613). I ask specifically about self-injurious behaviors, suicidal thoughts, suicidal plans or past attempts, and risk factors in the household such as guns and other weapons, prescription medications, and poisons. I also ask about use or abuse of alcohol and drugs, as well as other risk-taking behaviors such as high-speed driving and unprotected sex.
Particularly important in terms of acute suicidal risk is any event that the adolescent perceives as life-changing and irreversible—for example, abrupt loss of a significant romantic relationship, failure to achieve a highly desired goal (such as high grades for Aran), or some form of humiliation such as being bullied or publicly shamed. The risk of suicide after such events typically is acute but short-lived, so in a depressed adolescent, awareness of the importance of such an occurrence can be life-saving.
I always interview parents or other informants about their take on the patient’s mood and behaviors, usually separate from the adolescent. Parents can offer crucial details such as how much time a teen spends alone versus with friends or on other activities, and the progression of symptoms over time. It also is important to ask each parent about attitudes toward their child being on a medication and to address any expressed concerns. If parents describe a strikingly different presentation, I have everyone meet together to discuss those differences. This can also be a time to bring up issues that the adolescent and I agree parents need to know.

Table: Tips for Diagnosing Depression by Age Group
Click to view as full-sized PDF.
Depression in latency-age children
Amelia was a 10-year-old white female who came with her parents for evaluation because of falling grades and social withdrawal, worsening over the past 6 months. The parents initially denied any stressors in her life, but when she was out of earshot, confided that they were considering separation or divorce. Until recently, school had been easy and a source of pride for Amelia, but she now was less invested academically. She complained of not being able to sleep and of waking repeatedly throughout the night; she often napped in the late afternoon, sometimes for several hours. She had also been eating less and was not gaining weight, and often declined opportunities to play with friends. Her parents also reported that she was angry with them, complaining alternately that they didn’t care or were too intrusive. She had never talked about wanting to die; but sometimes, they found her crying in her room, and she never explained why.
On interview, Amelia presented as a thin, casually groomed child who insisted “everything is fine.” She admitted that she sometimes got upset with her parents and yelled at them, explaining, “They are too bossy.” She said her friends were often mean to her, which was why she got upset. She knew she was doing worse in school, stating, “The work is harder.” She cried once when asked about friends and again when asked about home, but quickly recovered. She firmly insisted she was not “depressed”; however, when we looked at a list of synonyms for depression, she said she was often “blue.”
Depressive symptoms in children from ages 6–12 tend to be fairly similar to adults. They are apt to appear sad, though they often lack words for describing their mood. As with Amelia, one important clinical task with kids this age is to work with them to find a word or phrase that best matches their mood and then use that term with them. A clinical tip is to have a list of synonyms for depression such as “sad,” “down,” “blue,” “moody,” “off,” and “irritated” that can study together. Kids this age can be quite concrete and may only endorse the term that “fits” them.
Like teens, children typically respond to their environment by being fine in some settings and distressed in others (CS Pataki and GA Carlson, Harvard Rev Psychiatry 1995;3(3):140–151). They are especially prone to somatic complaints and worries about their health and that of others. A depressed child might say things like “my stomach hurts when I think about school” or “sometimes my head hurts so bad I’m sure something is wrong with me.” Sleeping may be disrupted, with trouble getting to sleep and increased likelihood of awakening during the night or early in the morning. This is not a decreased need for sleep but an inability to get enough sleep, and you will often hear about napping in the afternoon, like with Amelia, or on long rides. Mood-congruent auditory and visual hallucinations occur in 20–25% of young children with severe depression (Carlson GA and Kashan JH, Amer J Psychiatry 1988;145(10):1222-1225). Tantrums and meltdowns also are common.
Children are highly sensitive to environmental strains and stresses, so I ask about the home environment. A remarkable number of parents who are having marital problems believe that their children are oblivious to the stress and uncertainty they are creating. Parents may not volunteer information about the marriage or other troubles within their family, such as chronic sibling squabbles, unless I ask. It’s also important to inquire about bullying or abuse from peers or adults, past or present.
Persistent depressive disorder (dysthymia) is especially prevalent in latency-age children. Such children have a negative take on the world and tend to expect the worst. It can be tempting to write such attitudes off as “temperament,” but research has shown that children with persistent depressive disorder have at least a 40% chance of developing a major depression within 2–3 years (Kovacs M et al, Arch Gen Psychiatry. 1984 41(7):643-9).
Depression in children under age 6
Juan was a 4-year-2-month old Hispanic male who came with his adoptive parents for assessment of chronic irritability, social withdrawal, poor appetite, and disrupted sleep. He had been separated from his biological mother at age 6 months and was in foster care until adopted by his parents at age 2. The parents had been told that his biological mother was neglectful but not abusive. He talked little when he first came into their home but quickly caught up with all milestones and seemed fine until about age 3, when he began to display the above symptoms.
Juan did well in preschool, getting along with teachers and peers. Parents reported that he had a low frustration tolerance, reacting with tantrums if he did not get a toy he wanted, then expressing feelings of guilt and saying he was “bad” once the tantrum ended. Testing showed that his language and motor skills were at or above age level. With the examiner, he played readily, but themes of the play were negative with bad outcomes such as people being hit by cars or falling off cliffs. Also, he showed little enthusiasm with the play and was quiet and soft-spoken with a subdued affect.
In the 1940s, Rene Spitz coined the term “anaclitic depression” to describe the reaction of infants under 1 year of age who were separated from their primary caregiver and placed in institutional care with minimal adult interaction (Spitz, Psychoanalytic Study Child 1946;2:113–117). Over the course of several months, they deteriorated both physically and emotionally and, after 5 to 6 months of such neglect, would develop appetite loss, weight loss, and diminished reactions.
More recent research has confirmed that depressive symptoms do occur in very young children (Luby, Amer J Psychiatry 2009;166(9):974–979), but there is some controversy about whether depression in the very young is the same disorder as that in older people. Key features include feeling and appearing sad most or all of the time, crying, being irritable and socially withdrawn, having somatic complaints with extreme fatigue, and feeling excessive guilt and shame. Parents are especially unlikely to consider depression as a problem in toddlers, so I ask specifically about these symptoms.
As with prepubertal children, environmental factors such as abuse or neglect or loss of a major caregiver may be key to the development of depression in very young children. In fact, for depressed children under age 6, abuse or neglect or both should be considered present until proven otherwise.
Summary
Assessing depression in children presents some challenges. It can take time to establish trust with the patient and gather vital information from other sources, children may lack the words to express their symptoms, and the symptoms themselves may be different from what one sees in adult depression. The table on page 3 provides a quick summary of key features of depression in young individuals. Because many parents may not consider depression as a cause for behavioral problems in children, it is crucial that clinicians ask questions of the youth and parents that will elicit symptoms, if present.
Child PsychiatryThe prevalence of depression increases markedly with age (Manepalli et al, Current Psychiatry 2011; 10:20–24), with rates of about 0.3% of preschoolers, 0.5%–3% of prepubertal children, 0.5%–6.5% of teenagers, and 10%–17% of adults. While adult depression is twice as common in women as in men, that ratio is nearly 1:1 in prepubertal children. In the early teen years, roughly correlating with the onset of puberty, though not necessarily associated with it, depression rates rise much more rapidly in females, so that the adult ratio of 1:2 is achieved by early-to-mid teens. While we don’t understand why, the bottom line is that young boys are as likely to have depression as young girls, while teen girls are twice as likely to be depressed as teen boys.
Depression in adolescents
Aran was a 15-year-old Asian male whose parents came to the U.S. as young adults. He was academically gifted and committed to scholarly pursuits, which his parents strongly encouraged. He was somewhat of a loner but had friends; his parents perceived him as being happy and eager to please. They were conservative about him spending time on social media and the Internet but he never complained, did expected household chores, and was involved in school-sponsored clubs.
The summer before his 10th grade year, Aran began to spend more time in his room, complained of being tired and started sleeping 10–12 hours a night. He seemed to be always hungry, gaining 12 pounds in 10 weeks, and became apathetic about previous interests such as video games. When school started, he took much longer doing his homework and had particular trouble with an advanced math class, getting his first-ever B+. He and his parents were both upset, and hired a tutor. However, when Aran took the final, he was convinced he failed it. That evening, he would not talk to his parents, did not eat supper, and went to his room. Worried, they entered his room, where they found him holding a sharp knife that he had taken from the kitchen. Aran began crying and tried to stab himself. His parents were able to wrest the knife from him and took him to the nearest emergency room, where he was assessed and hospitalized for suicidality.
One might assume that adolescents, being almost adults, would be most apt to present with adult-like signs and symptoms of depression. In fact, they are more likely to have atypical depressive symptoms such as increased appetite with weight gain and increased need for sleep (Pataki CS and Carlson GA, Harvard Rev Psychiatry 1995;3(3):140–151). In addition, their mood is less persistent and more reactive to environmental setting than is true for depressed adults. With friends and at school, they may seem happy and untroubled, only to appear deeply depressed when they are alone or at home, which can be particularly baffling—and frustrating—for parents.
When evaluating adolescents for depression, I usually begin by meeting briefly with the whole family, and then with the patient alone. Adolescents are often angry about having been forced to come see me but generally calm once parents leave. I start by exploring neutral or positive aspects of their life such as interests, what they like most about school, and favorite shows or hobbies. I then ask why they think their parents brought them to see me. I ask specifically about mood, using a variety of terms such as “down,” “irritable,” “sad,” “upset,” and “moody” and sticking to whatever term the adolescent endorses. I also ask about a series of symptoms and experiences common in adolescent depression (See the “Tips for Diagnosing Depression” table on page 3). Equally important are questions about how the teen feels about the possibility of taking a medication to help with depression and discussing any concerns.
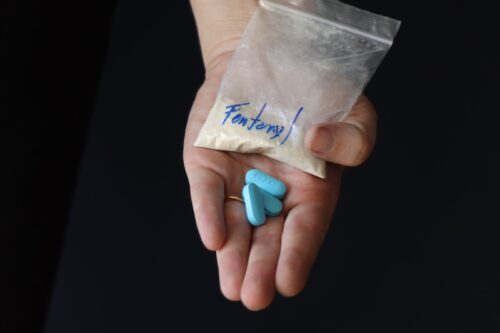
As with Aran’s scenario, depressed adolescents are at high risk for suicidal ideation. Some estimates suggest that as many as 60% of all adolescents think about killing themselves or that their family would be better off without them at least once during adolescence, though obviously for the vast majority it is idle speculation (VanderStoep A et al, Suicide Life Threat Behav 2009;39(6):599–613). I ask specifically about self-injurious behaviors, suicidal thoughts, suicidal plans or past attempts, and risk factors in the household such as guns and other weapons, prescription medications, and poisons. I also ask about use or abuse of alcohol and drugs, as well as other risk-taking behaviors such as high-speed driving and unprotected sex.
Particularly important in terms of acute suicidal risk is any event that the adolescent perceives as life-changing and irreversible—for example, abrupt loss of a significant romantic relationship, failure to achieve a highly desired goal (such as high grades for Aran), or some form of humiliation such as being bullied or publicly shamed. The risk of suicide after such events typically is acute but short-lived, so in a depressed adolescent, awareness of the importance of such an occurrence can be life-saving.
I always interview parents or other informants about their take on the patient’s mood and behaviors, usually separate from the adolescent. Parents can offer crucial details such as how much time a teen spends alone versus with friends or on other activities, and the progression of symptoms over time. It also is important to ask each parent about attitudes toward their child being on a medication and to address any expressed concerns. If parents describe a strikingly different presentation, I have everyone meet together to discuss those differences. This can also be a time to bring up issues that the adolescent and I agree parents need to know.

Table: Tips for Diagnosing Depression by Age Group
Click to view as full-sized PDF.
Depression in latency-age children
Amelia was a 10-year-old white female who came with her parents for evaluation because of falling grades and social withdrawal, worsening over the past 6 months. The parents initially denied any stressors in her life, but when she was out of earshot, confided that they were considering separation or divorce. Until recently, school had been easy and a source of pride for Amelia, but she now was less invested academically. She complained of not being able to sleep and of waking repeatedly throughout the night; she often napped in the late afternoon, sometimes for several hours. She had also been eating less and was not gaining weight, and often declined opportunities to play with friends. Her parents also reported that she was angry with them, complaining alternately that they didn’t care or were too intrusive. She had never talked about wanting to die; but sometimes, they found her crying in her room, and she never explained why.
On interview, Amelia presented as a thin, casually groomed child who insisted “everything is fine.” She admitted that she sometimes got upset with her parents and yelled at them, explaining, “They are too bossy.” She said her friends were often mean to her, which was why she got upset. She knew she was doing worse in school, stating, “The work is harder.” She cried once when asked about friends and again when asked about home, but quickly recovered. She firmly insisted she was not “depressed”; however, when we looked at a list of synonyms for depression, she said she was often “blue.”
Depressive symptoms in children from ages 6–12 tend to be fairly similar to adults. They are apt to appear sad, though they often lack words for describing their mood. As with Amelia, one important clinical task with kids this age is to work with them to find a word or phrase that best matches their mood and then use that term with them. A clinical tip is to have a list of synonyms for depression such as “sad,” “down,” “blue,” “moody,” “off,” and “irritated” that can study together. Kids this age can be quite concrete and may only endorse the term that “fits” them.
Like teens, children typically respond to their environment by being fine in some settings and distressed in others (CS Pataki and GA Carlson, Harvard Rev Psychiatry 1995;3(3):140–151). They are especially prone to somatic complaints and worries about their health and that of others. A depressed child might say things like “my stomach hurts when I think about school” or “sometimes my head hurts so bad I’m sure something is wrong with me.” Sleeping may be disrupted, with trouble getting to sleep and increased likelihood of awakening during the night or early in the morning. This is not a decreased need for sleep but an inability to get enough sleep, and you will often hear about napping in the afternoon, like with Amelia, or on long rides. Mood-congruent auditory and visual hallucinations occur in 20–25% of young children with severe depression (Carlson GA and Kashan JH, Amer J Psychiatry 1988;145(10):1222-1225). Tantrums and meltdowns also are common.
Children are highly sensitive to environmental strains and stresses, so I ask about the home environment. A remarkable number of parents who are having marital problems believe that their children are oblivious to the stress and uncertainty they are creating. Parents may not volunteer information about the marriage or other troubles within their family, such as chronic sibling squabbles, unless I ask. It’s also important to inquire about bullying or abuse from peers or adults, past or present.
Persistent depressive disorder (dysthymia) is especially prevalent in latency-age children. Such children have a negative take on the world and tend to expect the worst. It can be tempting to write such attitudes off as “temperament,” but research has shown that children with persistent depressive disorder have at least a 40% chance of developing a major depression within 2–3 years (Kovacs M et al, Arch Gen Psychiatry. 1984 41(7):643-9).
Depression in children under age 6
Juan was a 4-year-2-month old Hispanic male who came with his adoptive parents for assessment of chronic irritability, social withdrawal, poor appetite, and disrupted sleep. He had been separated from his biological mother at age 6 months and was in foster care until adopted by his parents at age 2. The parents had been told that his biological mother was neglectful but not abusive. He talked little when he first came into their home but quickly caught up with all milestones and seemed fine until about age 3, when he began to display the above symptoms.
Juan did well in preschool, getting along with teachers and peers. Parents reported that he had a low frustration tolerance, reacting with tantrums if he did not get a toy he wanted, then expressing feelings of guilt and saying he was “bad” once the tantrum ended. Testing showed that his language and motor skills were at or above age level. With the examiner, he played readily, but themes of the play were negative with bad outcomes such as people being hit by cars or falling off cliffs. Also, he showed little enthusiasm with the play and was quiet and soft-spoken with a subdued affect.
In the 1940s, Rene Spitz coined the term “anaclitic depression” to describe the reaction of infants under 1 year of age who were separated from their primary caregiver and placed in institutional care with minimal adult interaction (Spitz, Psychoanalytic Study Child 1946;2:113–117). Over the course of several months, they deteriorated both physically and emotionally and, after 5 to 6 months of such neglect, would develop appetite loss, weight loss, and diminished reactions.
More recent research has confirmed that depressive symptoms do occur in very young children (Luby, Amer J Psychiatry 2009;166(9):974–979), but there is some controversy about whether depression in the very young is the same disorder as that in older people. Key features include feeling and appearing sad most or all of the time, crying, being irritable and socially withdrawn, having somatic complaints with extreme fatigue, and feeling excessive guilt and shame. Parents are especially unlikely to consider depression as a problem in toddlers, so I ask specifically about these symptoms.
As with prepubertal children, environmental factors such as abuse or neglect or loss of a major caregiver may be key to the development of depression in very young children. In fact, for depressed children under age 6, abuse or neglect or both should be considered present until proven otherwise.
Summary
Assessing depression in children presents some challenges. It can take time to establish trust with the patient and gather vital information from other sources, children may lack the words to express their symptoms, and the symptoms themselves may be different from what one sees in adult depression. The table on page 3 provides a quick summary of key features of depression in young individuals. Because many parents may not consider depression as a cause for behavioral problems in children, it is crucial that clinicians ask questions of the youth and parents that will elicit symptoms, if present.
Issue Date: November 1, 2015
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)