Home » Foster Care and Child Psychiatry: A Primer
Foster Care and Child Psychiatry: A Primer
September 1, 2015
From The Carlat Child Psychiatry Report
Glen R. Elliott, PhD, MD
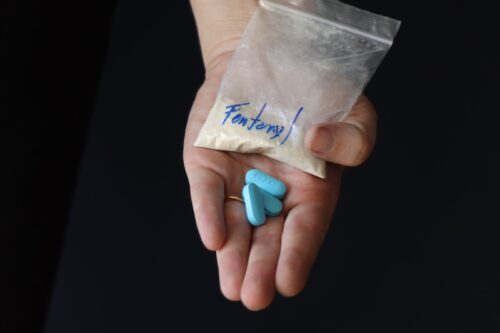
In this issue of CCPR we focus on the treatment of children in foster care systems. Nearly one in three of these children have significant psychiatric problems during their time in foster care—especially those related to trauma and neglect that brought them into the system (McMillen JC et al, J Am Acad Child Adolesc Psychiatry 2005;44(1):88–95). Recently, psychiatrists working with foster kids have been under fire for allegedly overusing medications, especially antipsychotics.
The articles in this issue will help practitioners answer questions such as: When do we use medications, and why, and what other options for treatment exist? In this introductory article, I’ll provide you with a brief primer on how foster care works, and how psychiatrists get involved.
What is Foster Care?
When children are in a tough home situation—whether involving abuse, neglect, or other circumstances—it’s not a given that they will end up in foster care. At least 25% go into what’s called “kinship care” (Child Welfare Information Gateway Kinship Care Resource; Winokur, M. Cochran Database System Review 2014 (1)). This means that the child goes to live with a relative or a family friend for a while, often in an informal arrangement that does not involve the courts or legal action. This is not foster care, because the child is not a “ward of the state.”
Foster care typically enters the picture when an untenable home situation comes to the attention of the police or a state agency such as child protective services (Schor EL Pediatr Clin North Am 1988;35(6):1241–1252). Sometimes, the parents call the authorities because they are concerned for their child’s well-being. Other times, someone else such as a teacher, physician, mental health worker, or neighbor reports concerns. When the situation is dire, police respond to a complaint and are dispatched to the home, often with a social worker. The child may then be taken into temporary protective custody with an organization such as a state’s department of social services or children’s shelter care system for 48–72 hours. After this, there is a confusing set of hearings that will vary from state to state. During these hearings, the child might be living with a temporary foster family or in a group home.
There are various reasons psychiatrists might need to know about this process. First, as a mandated reporter, you may be the one who contacts child protective services because of concerns about a child’s safety. Second, you may be asked to do an evaluation over the course of the hearings to determine whether placement outside the home is in the best interest of the child. If it is decided that the child should be returned to the current home environment, you may be asked to complete a reunification readiness assessment. Third, if you end up treating the child, some of the first records you review will be reports detailing the outcomes of the hearings.
Once the child is in the legal system, there are typically three hearings. First, there is an emergency detention hearing to decide if there are enough grounds to keep the child in protective custody while a more deliberate decision-making process occurs. Second, a jurisdictional hearing will take place usually within 2 weeks where the judge reviews all the evidence and decides if the allegations of abuse or neglect are true. Finally, if the judge agrees with the need for custody, there is a dispositional hearing. For this hearing, a social worker prepares a “case plan” that lays out the problem and a proposed solution. Often, a psychiatrist is asked to do a diagnostic evaluation and to recommend a treatment plan. Based on this hearing, the child might be placed in one of several situations. Options include not only being placed in a foster family home (what most typically think of as foster care, basically living with strangers) but also being fostered with relatives or living in a group home or a residential care facility, the latter places differing mainly by the size of the foster population. There are also short-term emergency shelters when more permanent placement is not immediately available. The intent of the system is to place the child in the least restrictive setting compatible with good care, with the ultimate goal, when feasible, of returning the child as quickly as possible back to the parents or legal guardians.
The Foster Family
In 2013 (the most current data available), the total number of children and adolescents in foster care was just over 400,000, with 15% under age 2 and 25% between the ages of 14 through 17 (AFCARS Report #22).
While specific rules vary across states, foster parents must have state licensure and receive training before taking responsibility for a child (Foster Care Statistics 2013). They are also screened in other ways, including age, income, suitability of housing, and absence of a criminal record. Foster parents receive reimbursement, usually a per-diem rate per child in the range of $20–$25/day, depending on the state (the amount increases if more intensive psychiatric or medical conditions exist). As a clinician, you will want to have a sense of who the child’s foster family is so that you can assess the appropriateness of placement and adequacy of parenting, just as you would with any other child or adolescent.
Foster Care and Psychiatric Treatment
Foster care children can have an array of behavioral problems and specific psychiatric disorders. The process of being taken out of one’s home and separated from parents and siblings is stressful, even in the absence of a specific traumatic event. Since many children are removed by child protective services because of neglect, abuse, or unsafe living situations, foster care children may have complex reactions of relief combined with guilt and feelings of abandonment. One study of foster adolescents (McMillen JC et al, J Am Acad Child Adolesc Psychiatry 2005;44(1):88–95) found a 32% prevalence of lifetime psychiatric disorders, and 10% of those surveyed met criteria for both an internalizing disorder such as major depression, PTSD, or mania and an externalizing disorder such as ADHD or some other disruptive behavior disorder. In this study, the best predictor of having a psychiatric disorder was the number of different types of maltreatment the individual had experienced.
One of the challenges of working with children in foster care is that there is often no one who knows the child well or can report on the longitudinal course of symptoms. Many children have jumped from provider to provider and may be taking multiple psychiatric medications. If you are a new provider caring for such a child, get your own history of symptoms before continuing to treat apparent mania or psychosis that may actually be complex PTSD, depression, or simply a child’s acting out in a maladaptive attempt to gain control. Some children believe that if they act badly enough in the foster home they will be returned to their parents. Alternatively, they may anticipate rejection by the foster family and act out to elicit the expected rejection—to avoid getting attached to the new caregivers and then being disappointed.
The bottom line is that foster care children are likely to have significant psychiatric issues, and the best treatment includes a coordinated team of foster parents, mental health professionals, and child welfare services staff such as social workers and court-appointed special advocates. We’ll get into the details of treatment recommendations in the other articles in this issue.

Table: Antipsychotics Potentially Used in Children
Click here for full-size table.
Basic Principles for Medication Use in Foster Children
Child PsychiatryThe articles in this issue will help practitioners answer questions such as: When do we use medications, and why, and what other options for treatment exist? In this introductory article, I’ll provide you with a brief primer on how foster care works, and how psychiatrists get involved.
What is Foster Care?
When children are in a tough home situation—whether involving abuse, neglect, or other circumstances—it’s not a given that they will end up in foster care. At least 25% go into what’s called “kinship care” (Child Welfare Information Gateway Kinship Care Resource; Winokur, M. Cochran Database System Review 2014 (1)). This means that the child goes to live with a relative or a family friend for a while, often in an informal arrangement that does not involve the courts or legal action. This is not foster care, because the child is not a “ward of the state.”
Foster care typically enters the picture when an untenable home situation comes to the attention of the police or a state agency such as child protective services (Schor EL Pediatr Clin North Am 1988;35(6):1241–1252). Sometimes, the parents call the authorities because they are concerned for their child’s well-being. Other times, someone else such as a teacher, physician, mental health worker, or neighbor reports concerns. When the situation is dire, police respond to a complaint and are dispatched to the home, often with a social worker. The child may then be taken into temporary protective custody with an organization such as a state’s department of social services or children’s shelter care system for 48–72 hours. After this, there is a confusing set of hearings that will vary from state to state. During these hearings, the child might be living with a temporary foster family or in a group home.
There are various reasons psychiatrists might need to know about this process. First, as a mandated reporter, you may be the one who contacts child protective services because of concerns about a child’s safety. Second, you may be asked to do an evaluation over the course of the hearings to determine whether placement outside the home is in the best interest of the child. If it is decided that the child should be returned to the current home environment, you may be asked to complete a reunification readiness assessment. Third, if you end up treating the child, some of the first records you review will be reports detailing the outcomes of the hearings.
Once the child is in the legal system, there are typically three hearings. First, there is an emergency detention hearing to decide if there are enough grounds to keep the child in protective custody while a more deliberate decision-making process occurs. Second, a jurisdictional hearing will take place usually within 2 weeks where the judge reviews all the evidence and decides if the allegations of abuse or neglect are true. Finally, if the judge agrees with the need for custody, there is a dispositional hearing. For this hearing, a social worker prepares a “case plan” that lays out the problem and a proposed solution. Often, a psychiatrist is asked to do a diagnostic evaluation and to recommend a treatment plan. Based on this hearing, the child might be placed in one of several situations. Options include not only being placed in a foster family home (what most typically think of as foster care, basically living with strangers) but also being fostered with relatives or living in a group home or a residential care facility, the latter places differing mainly by the size of the foster population. There are also short-term emergency shelters when more permanent placement is not immediately available. The intent of the system is to place the child in the least restrictive setting compatible with good care, with the ultimate goal, when feasible, of returning the child as quickly as possible back to the parents or legal guardians.
The Foster Family
In 2013 (the most current data available), the total number of children and adolescents in foster care was just over 400,000, with 15% under age 2 and 25% between the ages of 14 through 17 (AFCARS Report #22).
While specific rules vary across states, foster parents must have state licensure and receive training before taking responsibility for a child (Foster Care Statistics 2013). They are also screened in other ways, including age, income, suitability of housing, and absence of a criminal record. Foster parents receive reimbursement, usually a per-diem rate per child in the range of $20–$25/day, depending on the state (the amount increases if more intensive psychiatric or medical conditions exist). As a clinician, you will want to have a sense of who the child’s foster family is so that you can assess the appropriateness of placement and adequacy of parenting, just as you would with any other child or adolescent.
Foster Care and Psychiatric Treatment
Foster care children can have an array of behavioral problems and specific psychiatric disorders. The process of being taken out of one’s home and separated from parents and siblings is stressful, even in the absence of a specific traumatic event. Since many children are removed by child protective services because of neglect, abuse, or unsafe living situations, foster care children may have complex reactions of relief combined with guilt and feelings of abandonment. One study of foster adolescents (McMillen JC et al, J Am Acad Child Adolesc Psychiatry 2005;44(1):88–95) found a 32% prevalence of lifetime psychiatric disorders, and 10% of those surveyed met criteria for both an internalizing disorder such as major depression, PTSD, or mania and an externalizing disorder such as ADHD or some other disruptive behavior disorder. In this study, the best predictor of having a psychiatric disorder was the number of different types of maltreatment the individual had experienced.
One of the challenges of working with children in foster care is that there is often no one who knows the child well or can report on the longitudinal course of symptoms. Many children have jumped from provider to provider and may be taking multiple psychiatric medications. If you are a new provider caring for such a child, get your own history of symptoms before continuing to treat apparent mania or psychosis that may actually be complex PTSD, depression, or simply a child’s acting out in a maladaptive attempt to gain control. Some children believe that if they act badly enough in the foster home they will be returned to their parents. Alternatively, they may anticipate rejection by the foster family and act out to elicit the expected rejection—to avoid getting attached to the new caregivers and then being disappointed.
The bottom line is that foster care children are likely to have significant psychiatric issues, and the best treatment includes a coordinated team of foster parents, mental health professionals, and child welfare services staff such as social workers and court-appointed special advocates. We’ll get into the details of treatment recommendations in the other articles in this issue.

Table: Antipsychotics Potentially Used in Children
Click here for full-size table.
Basic Principles for Medication Use in Foster Children
- Make sure there is a larger treatment plan in place, including psychosocial approaches.
- Review as many collateral documents as you can, such as court reports, prior medical and psychiatric records, and the individualized education program (IEP).
- Identify and carefully document diagnoses and specific target symptoms.
- Consider whether existing medication therapy may be exacerbating current symptoms.
- Prioritize specific target symptoms that will be targeted by the medication (most problematic and most recent symptoms having greatest priority); set reasonable goals and make one pharmacologic intervention at a time, if possible.
- Monitor therapeutic response regularly; taper/discontinue if no benefit.
- Monitor side effects regularly; consider alternatives if a child is experiencing side effects.
- When possible, choose agents with FDA indications for pediatric use, use lowest effective doses, attempt sequential monotherapies before initiating polypharmacy, and make periodic assessments to determine whether medication is still indicated.
- Available evidence to support the use of medication in preschool-aged children is extremely limited; non-pharmacologic interventions should be tried first (Gleason MM et al, J Am Acad Child Adolesc Psychiatry 2007;46(12):1532–1572)
- Medications should not be used as disciplinary measures or chemical restraint, nor should they be a condition for placement of foster children.
KEYWORDS antipsychotics child-psychiatry free_articles practice-tools-and-tips psychopharmacology_tips psychotherapy ptsd
Issue Date: September 1, 2015
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)