Home » Hallucinations in Children and Adolescents
Hallucinations in Children and Adolescents
July 1, 2014
From The Carlat Child Psychiatry Report
Jerome Fialkov, MD
Hallucinations are relatively common in children. Two-thirds of children ages nine to 11 have had at least one psychotic-like experience, including hallucinations.
Studies of large pediatric samples document an eight percent hallucination prevalence rate in children (McGee R et al, JAACAP 2000;39(1):12–13). The vast majority of hallucinations in the general pediatric population are transient and resolve spontaneously. In approximately 50% to 95% of cases, hallucinations discontinue after a few weeks or months (Rubio JM et al, Schizophr Res 2012;138(2–3):249–254).
Hallucinations can be scary for parents and other caregivers, but they don’t usually signal major psychopathology and are mostly associated with anxiety and stressful events. In this article, we’ll explore some of the causes of psychotic and non-psychotic hallucinations in children and adolescents and appropriate interventions for them.
What Exactly is a Hallucination?
Sir Thomas Browne, the 17th century physician, coined the term hallucination in 1646, deriving it from the Latin alucinari meaning “to wander in the mind.” DSM-IV defines a hallucination “as a sensory perception, which has the compelling sense of reality of a true perception, but occurs without external stimulation of the relevant sensory organ.”
Hallucinations are distortions in sensory perception in any or all of the five human senses. The most common hallucinations are auditory and visual, but olfactory, gustatory (taste), tactile, proprioceptive, and somatic also occur. Hallucinations may be mood-congruent or incongruent.
“True” hallucinations must be distinguished from perceptual distortions such as illusions or vivid imaginings, and other phenomena such as obsessions, compulsions, dissociative phenomena, pseudohallucinations, and borderline syndrome of childhood (Lewis M, Child Adolesc Psychiatr Clin North Am 1994;3:31–43). In addition, hallucinations may be feigned by children and adolescents, often to get themselves out of situations with the law, their parents, peers, and others in authority (Resnick PJ. In: Rogers R, ed. Clinical Assessment of Malingering and Deception. 2nd ed. New York: Guilford Press;1997:p 47–67).
An hallucination is meaningful only after a child has learned to distinguish between his/her internal world and external reality. There is disagreement as to the age when this distinction can be made, but it is thought that a normal child of average intelligence is fully able to distinguish between fantasy and reality by the age of three (Piaget J. The child’s construction of reality. London: Routledge and Kegan;1995).
Imaginary companions, sometimes described as “hallucination-like phenomena,” differ from hallucinations in that they can often be evoked by the child at will (in contrast with the involuntary nature of hallucinations), and may typically function as playing partners associated with positive emotions. However, “noncompliant imaginary companions” exist, and are resistant to the host child’s control (Taylor MA. Imaginary Companions and the Children Who Create Them. UK: Oxford University Press;1999).
Other related phenomena observed during the developmental period include sleep-related hallucinations. Hypnagogic hallucinations, occurring immediately before falling asleep, and hypnopompic hallucinations, occurring during the transition from sleep to wakefulness, are reported in 25% and 18% of the general population, respectively, but decline with age into adulthood. These may be part of a disabling childhood sleep disorder such as narcolepsy with cataplexy (Dauvilliers Y et al, Lancet 2007;369(9560):499–511).
Pseudohallucinations are mental images which, although clear and vivid, lack the substantiality of perceptions. They are seen in full consciousness, known to be not real perceptions, are not located in objective space, but in subjective space, and are dependent on the individual’s insight. They may be experienced by hysterical or attention-seeking personalities.
Psychiatric Causes and Comorbidities
Many non-psychotic hallucinations are associated with periods of anxiety and stress, and disappear when the stressful situation is resolved (Mertin P & Hartwig S, Child Adolesc Ment Health 2004;9(1):9–14).
Illusions are misperceptions or misinterpretations of real external stimuli and may occur in delirium, depression with delusions of guilt, and/or be self-referential. These may manifest as fantastic illusions in which a child or adolescent describes extraordinary modifications of his environment (eg, he looks in a mirror and instead of seeing his own head, sees that of a pig); or pareidolia—illusions that occur without the patient making any effort, which may be due to excessive fantasy thinking and a vivid visual imagery.
Several studies have demonstrated that experiencing childhood trauma is a risk factor for psychosis and hallucinations. A positive association has been found for sexual abuse, physical abuse, emotional abuse, bullying, or neglect, but not parental death (Varese F et al, Schizophr Bull 2012;38:661–671). A subsequent study confirmed that those with high sexual abuse scores were two to four times more likely to develop adult psychosis (Thompson AD et al, Schizophr Bull 2014;40(3):697–706).
Mood disorders can often present with accompanying psychotic features, including hallucinations (Edelsohn GA, Am J Psychiatry 2006;163(5):781–785). Research in clinical populations demonstrated that 11- to 15-year-old patients who reported psychotic experiences had, on average, three diagnosable DSM-IV, Axis I disorders. In these cases, psychotic symptoms predict more severe psychopathology (Kelleher et al, Br J Psychiatry 2012;201(1):26–32).
There is a significant relationship between psychotic hallucinations and suicidal behavior. Adolescents with a diagnosis of major depression disorder (MDD) who report psychotic experiences had a 14-fold increase in suicide plans or attempts compared to adolescents with the same diagnosis who did not report psychotic experiences (Kelleher I et al, Arch Gen Psychiatry 2012;69(12):1277–1283).
Non-psychotic children who hallucinate may have diagnoses of ADHD (22%), MDD, (34%), or disruptive behavior disorders (21%) (Edelsohn GA et al, Ann N Y Acad Sci 2003;1008:261–264).
What About Schizophrenia in Childhood and Adolescence?
Childhood-onset schizophrenia is extremely rare, and the majority of children experiencing hallucinations do not progress to that level of psychiatric disturbance. The likelihood of schizophrenia occurring before 13 years of age is one in 30,000 (Jardri R et al, Schizophr Bull 2014;40(suppl 4):S221–S232). Schizophrenia can be reliably diagnosed in children and it is neurobiologically, diagnostically, and physiologically continuous with the adult disorder.
Nearly all of the National Institute of Mental Health (NIMH) childhood-onset schizophrenia cohort had high rates of hallucinations across all sensory modalities. These were predominantly significant auditory hallucinations; but there was also a high rate of visual hallucinations (80%), along with tactile (60%) and olfactory (30%) hallucinations associated with them. Those with visual hallucinations showed a significant association with lower IQ and early age of psychosis onset (David CN et al, JAACAP 2011; 50(7):681–686).
Medical Causes of Hallucinations
Medications, substance use, and organic and metabolic disorders can all cause hallucinations. Medical causes include electrolyte disturbances, metabolic disorders, fever, and serious infections.
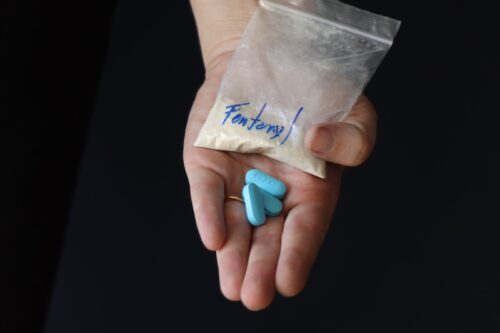
Some hallucinations may be regarded as manifestations of delirium, and may be due to medication such as steroids and anticholinergics, methylphenidate, and/or illicit substances including cannabis, lysergic acid diethylamide (LSD), cocaine, amphetamine, methamphetamine, MDMA (ecstasy), opiates, and synthetic drugs.
Visual, gustatory, and olfactory hallucinations are highly suggestive of a medical- or substance-related origin. Substance-induced hallucinations should be suspected if an individual shows acute onset of hallucinations, dilated pupils, extreme agitation or drowsiness, and other signs of intoxication.
Children with seizure disorders can experience hallucinations that may be somatosensory, visual (occipital lobe focus), auditory, olfactory (uncinate, complex partial), or gustatory. Complex partial seizures, especially those with a temporal focus, may be associated with interictal psychotic symptoms of delusions, hallucinations, and unusual preoccupations. The hallucinations may be unformed (flashing lights or rushing noises) or formed (images, spoken word or music) and could be part of the aura arising from the temporal lobe (dream-like, flashbacks).
Perceptual sensory distortions may be due to central lesions affecting the posterior part of the temporal lobe. These may include hyperesthesia and hypoesthesia (over- or undersensitivity to stimuli, respectively) and visual distortions, such as micropsia (seeing things as smaller than they are) and the opposite, macropsia.
Migraines occur in approximately five percent of prepubertal children, and often are comorbid with affective and anxiety disorders. Hallucinations associated with migraine commonly are visual, but gustatory, olfactory, and auditory hallucinations also can occur with or without headaches. Any hallucination associated with headaches should be investigated neurologically.
Assessment of the Child with Hallucinations
Children or adolescents with hallucinations should undergo a thorough evaluation that includes both a physical examination to rule out medical causes and psychological assessment to identify psychopathological, psychosocial, and cultural factors associated with their experiences.
When interviewing children, one should bear in mind that they are highly suggestible, may answer questions in the affirmative to get attention or to please the interviewer, may not fully or partially understand what is being asked, and may blame their misbehavior on voices to escape punishment. In addition, they may not distinguish between fantasies, dreams, feelings, and internal conflicts.
The workup must include ruling out substance ingestions and medical and neurological causes. Hallucinations must be evaluated in the context of other features of psychosis, such as onset, frequency, severity, and chronicity. Remember, too, to assess for trauma and sexual and physical abuse, as perceptual disturbances are common in these children.
Children with hallucinations require immediate medical intervention to identify the cause and to provide appropriate treatment. They may need laboratory tests such as serum electrolytes, complete blood count with differential, liver, renal and thyroid function tests, toxicology screens, blood alcohol level, serum levels of mood stabilizers (valproate, lithium, carbamazepine), and of neuroleptics. They may need brain imaging to rule out head injuries and other organic causes of delirium.
Careful monitoring of weight, blood pressure, pulse rate, and height, as well as fasting blood sugar, lipid levels, and thyroid and renal functions are necessary depending on medications the child is prescribed. Contact with key adults is critical, and efforts should be made to obtain consent of release of information.
Treatment of Hallucinations
Often, hallucinations are transient, harmless, and do not require treatment. However, early identification and treatment, when warranted, is imperative. Duration of untreated psychosis (DUP) is a primary predictor of treatment response in first admission patients, and longer DUP corresponds to poorer prognosis in children.
Several assessment scales for early identification of psychosis exist but are unreliable, and other rating scales have not been standardized for use in children younger than 14. However, some rating scales to monitor progress should be implemented on a regular basis when the child comes for treatment.
Patients with underlying depression, anxiety, or PTSD may need psychotherapy or antidepressants. Antipsychotics should be used with caution in this group, although they might be appropriate for children confirmed to be in the prodromal phase. [Eds note: see the interview on page 1 for more on diagnosis of prodromal states.]
Premature labeling of schizophrenia and the stigma that goes with it can have a long-term damaging effect. Although, contrarily, early intervention for confirmed schizophrenia is essential to dampen the effects of early poor prognosis of the condition.
Children with schizophrenia require multimodal care, including social skills training, a supportive environment, and a structured individualized special education program. Supportive psychotherapy can reinforce reality testing and help the child monitor for warning symptoms of impending relapse.
Cognitive behavioral therapy (CBT) has been used successfully and may help improve coping with schizophrenia and monitoring of beliefs and attributions. In addition, CBT has been shown to slow progression to psychosis in ultra-high-risk patients and reduces positive symptoms.
Olanzapine (Zyprexa), risperidone (Risperdal), and CBT have been found superior to case management and supportive psychotherapy in preventing psychosis after six months of treatment, but this difference was not maintained at six months of follow-up (McGorry et al, Arch Gen Psychiatry 2002;59(10):921–928)
Research has demonstrated some benefits of omega-3 fatty acids augmenting antipsychotic medication (Amminger GP et al, Arch Gen Psychiatry 2010;67(2):146–154). Further treatment can help children develop coping strategies to control auditory hallucinations, such as humming, listening to music, reading (forward and backward), talking to others, exercising, singing, medication, and ignoring the voices.
Pervasive problems of the child with schizophrenia requires a team approach involving nursing, speech and language therapy, occupational therapy, and physical therapy, while a case manager may facilitate care. A psychologist is an essential part of the evaluation and treatment team for a child with schizophrenia (Joshi PT & Towbin KE. Psychosis in Childhood and its Management. In: Neuropsychopharmacology: The Fifth Generation of Progress. Davis KL et al, eds. Baltimore, MD:Lippincott;2002).
CCPR’s Verdict: Hallucinations are symptoms, not a diagnosis, and can have a developmental, neurologic, metabolic or psychiatric basis. Visual, gustatory, and olfactory hallucinations suggest a medical- or substance-related origin. Schizophrenia is rare before age 13 and should be diagnosed only if prominent delusions and hallucinations are present at least a month.
Child PsychiatryStudies of large pediatric samples document an eight percent hallucination prevalence rate in children (McGee R et al, JAACAP 2000;39(1):12–13). The vast majority of hallucinations in the general pediatric population are transient and resolve spontaneously. In approximately 50% to 95% of cases, hallucinations discontinue after a few weeks or months (Rubio JM et al, Schizophr Res 2012;138(2–3):249–254).
Hallucinations can be scary for parents and other caregivers, but they don’t usually signal major psychopathology and are mostly associated with anxiety and stressful events. In this article, we’ll explore some of the causes of psychotic and non-psychotic hallucinations in children and adolescents and appropriate interventions for them.
What Exactly is a Hallucination?
Sir Thomas Browne, the 17th century physician, coined the term hallucination in 1646, deriving it from the Latin alucinari meaning “to wander in the mind.” DSM-IV defines a hallucination “as a sensory perception, which has the compelling sense of reality of a true perception, but occurs without external stimulation of the relevant sensory organ.”
Hallucinations are distortions in sensory perception in any or all of the five human senses. The most common hallucinations are auditory and visual, but olfactory, gustatory (taste), tactile, proprioceptive, and somatic also occur. Hallucinations may be mood-congruent or incongruent.
“True” hallucinations must be distinguished from perceptual distortions such as illusions or vivid imaginings, and other phenomena such as obsessions, compulsions, dissociative phenomena, pseudohallucinations, and borderline syndrome of childhood (Lewis M, Child Adolesc Psychiatr Clin North Am 1994;3:31–43). In addition, hallucinations may be feigned by children and adolescents, often to get themselves out of situations with the law, their parents, peers, and others in authority (Resnick PJ. In: Rogers R, ed. Clinical Assessment of Malingering and Deception. 2nd ed. New York: Guilford Press;1997:p 47–67).
An hallucination is meaningful only after a child has learned to distinguish between his/her internal world and external reality. There is disagreement as to the age when this distinction can be made, but it is thought that a normal child of average intelligence is fully able to distinguish between fantasy and reality by the age of three (Piaget J. The child’s construction of reality. London: Routledge and Kegan;1995).
Imaginary companions, sometimes described as “hallucination-like phenomena,” differ from hallucinations in that they can often be evoked by the child at will (in contrast with the involuntary nature of hallucinations), and may typically function as playing partners associated with positive emotions. However, “noncompliant imaginary companions” exist, and are resistant to the host child’s control (Taylor MA. Imaginary Companions and the Children Who Create Them. UK: Oxford University Press;1999).
Other related phenomena observed during the developmental period include sleep-related hallucinations. Hypnagogic hallucinations, occurring immediately before falling asleep, and hypnopompic hallucinations, occurring during the transition from sleep to wakefulness, are reported in 25% and 18% of the general population, respectively, but decline with age into adulthood. These may be part of a disabling childhood sleep disorder such as narcolepsy with cataplexy (Dauvilliers Y et al, Lancet 2007;369(9560):499–511).
Pseudohallucinations are mental images which, although clear and vivid, lack the substantiality of perceptions. They are seen in full consciousness, known to be not real perceptions, are not located in objective space, but in subjective space, and are dependent on the individual’s insight. They may be experienced by hysterical or attention-seeking personalities.
Psychiatric Causes and Comorbidities
Many non-psychotic hallucinations are associated with periods of anxiety and stress, and disappear when the stressful situation is resolved (Mertin P & Hartwig S, Child Adolesc Ment Health 2004;9(1):9–14).
Illusions are misperceptions or misinterpretations of real external stimuli and may occur in delirium, depression with delusions of guilt, and/or be self-referential. These may manifest as fantastic illusions in which a child or adolescent describes extraordinary modifications of his environment (eg, he looks in a mirror and instead of seeing his own head, sees that of a pig); or pareidolia—illusions that occur without the patient making any effort, which may be due to excessive fantasy thinking and a vivid visual imagery.
Several studies have demonstrated that experiencing childhood trauma is a risk factor for psychosis and hallucinations. A positive association has been found for sexual abuse, physical abuse, emotional abuse, bullying, or neglect, but not parental death (Varese F et al, Schizophr Bull 2012;38:661–671). A subsequent study confirmed that those with high sexual abuse scores were two to four times more likely to develop adult psychosis (Thompson AD et al, Schizophr Bull 2014;40(3):697–706).
Mood disorders can often present with accompanying psychotic features, including hallucinations (Edelsohn GA, Am J Psychiatry 2006;163(5):781–785). Research in clinical populations demonstrated that 11- to 15-year-old patients who reported psychotic experiences had, on average, three diagnosable DSM-IV, Axis I disorders. In these cases, psychotic symptoms predict more severe psychopathology (Kelleher et al, Br J Psychiatry 2012;201(1):26–32).
There is a significant relationship between psychotic hallucinations and suicidal behavior. Adolescents with a diagnosis of major depression disorder (MDD) who report psychotic experiences had a 14-fold increase in suicide plans or attempts compared to adolescents with the same diagnosis who did not report psychotic experiences (Kelleher I et al, Arch Gen Psychiatry 2012;69(12):1277–1283).
Non-psychotic children who hallucinate may have diagnoses of ADHD (22%), MDD, (34%), or disruptive behavior disorders (21%) (Edelsohn GA et al, Ann N Y Acad Sci 2003;1008:261–264).
What About Schizophrenia in Childhood and Adolescence?
Childhood-onset schizophrenia is extremely rare, and the majority of children experiencing hallucinations do not progress to that level of psychiatric disturbance. The likelihood of schizophrenia occurring before 13 years of age is one in 30,000 (Jardri R et al, Schizophr Bull 2014;40(suppl 4):S221–S232). Schizophrenia can be reliably diagnosed in children and it is neurobiologically, diagnostically, and physiologically continuous with the adult disorder.
Nearly all of the National Institute of Mental Health (NIMH) childhood-onset schizophrenia cohort had high rates of hallucinations across all sensory modalities. These were predominantly significant auditory hallucinations; but there was also a high rate of visual hallucinations (80%), along with tactile (60%) and olfactory (30%) hallucinations associated with them. Those with visual hallucinations showed a significant association with lower IQ and early age of psychosis onset (David CN et al, JAACAP 2011; 50(7):681–686).
Medical Causes of Hallucinations
Medications, substance use, and organic and metabolic disorders can all cause hallucinations. Medical causes include electrolyte disturbances, metabolic disorders, fever, and serious infections.
Some hallucinations may be regarded as manifestations of delirium, and may be due to medication such as steroids and anticholinergics, methylphenidate, and/or illicit substances including cannabis, lysergic acid diethylamide (LSD), cocaine, amphetamine, methamphetamine, MDMA (ecstasy), opiates, and synthetic drugs.
Visual, gustatory, and olfactory hallucinations are highly suggestive of a medical- or substance-related origin. Substance-induced hallucinations should be suspected if an individual shows acute onset of hallucinations, dilated pupils, extreme agitation or drowsiness, and other signs of intoxication.
Children with seizure disorders can experience hallucinations that may be somatosensory, visual (occipital lobe focus), auditory, olfactory (uncinate, complex partial), or gustatory. Complex partial seizures, especially those with a temporal focus, may be associated with interictal psychotic symptoms of delusions, hallucinations, and unusual preoccupations. The hallucinations may be unformed (flashing lights or rushing noises) or formed (images, spoken word or music) and could be part of the aura arising from the temporal lobe (dream-like, flashbacks).
Perceptual sensory distortions may be due to central lesions affecting the posterior part of the temporal lobe. These may include hyperesthesia and hypoesthesia (over- or undersensitivity to stimuli, respectively) and visual distortions, such as micropsia (seeing things as smaller than they are) and the opposite, macropsia.
Migraines occur in approximately five percent of prepubertal children, and often are comorbid with affective and anxiety disorders. Hallucinations associated with migraine commonly are visual, but gustatory, olfactory, and auditory hallucinations also can occur with or without headaches. Any hallucination associated with headaches should be investigated neurologically.
Assessment of the Child with Hallucinations
Children or adolescents with hallucinations should undergo a thorough evaluation that includes both a physical examination to rule out medical causes and psychological assessment to identify psychopathological, psychosocial, and cultural factors associated with their experiences.
When interviewing children, one should bear in mind that they are highly suggestible, may answer questions in the affirmative to get attention or to please the interviewer, may not fully or partially understand what is being asked, and may blame their misbehavior on voices to escape punishment. In addition, they may not distinguish between fantasies, dreams, feelings, and internal conflicts.
The workup must include ruling out substance ingestions and medical and neurological causes. Hallucinations must be evaluated in the context of other features of psychosis, such as onset, frequency, severity, and chronicity. Remember, too, to assess for trauma and sexual and physical abuse, as perceptual disturbances are common in these children.
Children with hallucinations require immediate medical intervention to identify the cause and to provide appropriate treatment. They may need laboratory tests such as serum electrolytes, complete blood count with differential, liver, renal and thyroid function tests, toxicology screens, blood alcohol level, serum levels of mood stabilizers (valproate, lithium, carbamazepine), and of neuroleptics. They may need brain imaging to rule out head injuries and other organic causes of delirium.
Careful monitoring of weight, blood pressure, pulse rate, and height, as well as fasting blood sugar, lipid levels, and thyroid and renal functions are necessary depending on medications the child is prescribed. Contact with key adults is critical, and efforts should be made to obtain consent of release of information.
Treatment of Hallucinations
Often, hallucinations are transient, harmless, and do not require treatment. However, early identification and treatment, when warranted, is imperative. Duration of untreated psychosis (DUP) is a primary predictor of treatment response in first admission patients, and longer DUP corresponds to poorer prognosis in children.
Several assessment scales for early identification of psychosis exist but are unreliable, and other rating scales have not been standardized for use in children younger than 14. However, some rating scales to monitor progress should be implemented on a regular basis when the child comes for treatment.
Patients with underlying depression, anxiety, or PTSD may need psychotherapy or antidepressants. Antipsychotics should be used with caution in this group, although they might be appropriate for children confirmed to be in the prodromal phase. [Eds note: see the interview on page 1 for more on diagnosis of prodromal states.]
Premature labeling of schizophrenia and the stigma that goes with it can have a long-term damaging effect. Although, contrarily, early intervention for confirmed schizophrenia is essential to dampen the effects of early poor prognosis of the condition.
Children with schizophrenia require multimodal care, including social skills training, a supportive environment, and a structured individualized special education program. Supportive psychotherapy can reinforce reality testing and help the child monitor for warning symptoms of impending relapse.
Cognitive behavioral therapy (CBT) has been used successfully and may help improve coping with schizophrenia and monitoring of beliefs and attributions. In addition, CBT has been shown to slow progression to psychosis in ultra-high-risk patients and reduces positive symptoms.
Olanzapine (Zyprexa), risperidone (Risperdal), and CBT have been found superior to case management and supportive psychotherapy in preventing psychosis after six months of treatment, but this difference was not maintained at six months of follow-up (McGorry et al, Arch Gen Psychiatry 2002;59(10):921–928)
Research has demonstrated some benefits of omega-3 fatty acids augmenting antipsychotic medication (Amminger GP et al, Arch Gen Psychiatry 2010;67(2):146–154). Further treatment can help children develop coping strategies to control auditory hallucinations, such as humming, listening to music, reading (forward and backward), talking to others, exercising, singing, medication, and ignoring the voices.
Pervasive problems of the child with schizophrenia requires a team approach involving nursing, speech and language therapy, occupational therapy, and physical therapy, while a case manager may facilitate care. A psychologist is an essential part of the evaluation and treatment team for a child with schizophrenia (Joshi PT & Towbin KE. Psychosis in Childhood and its Management. In: Neuropsychopharmacology: The Fifth Generation of Progress. Davis KL et al, eds. Baltimore, MD:Lippincott;2002).
CCPR’s Verdict: Hallucinations are symptoms, not a diagnosis, and can have a developmental, neurologic, metabolic or psychiatric basis. Visual, gustatory, and olfactory hallucinations suggest a medical- or substance-related origin. Schizophrenia is rare before age 13 and should be diagnosed only if prominent delusions and hallucinations are present at least a month.
KEYWORDS child-psychiatry
Issue Date: July 1, 2014
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)