Home » Approach to the Child with Intellectual Disability
Approach to the Child with Intellectual Disability
October 1, 2010
From The Carlat Child Psychiatry Report
Caroline Fisher, PhD, MD.
I first met Christina when she was 14. She had been diagnosed with borderline personality disorder and bipolar disorder. She had blown out of four private schools in the area, not for grades but for bad behavior. She was getting into physical fights with her siblings, drinking, and smoking marijuana.
“My parents hate me,” she said. In reviewing her records, I saw that she’d tried just about every medication in the pharmacy, it seemed, with almost no effect. Because I was at a loss as to what else to do, I started over with diagnosis: mood (fine), anxiety (denies), sleep (fine), social relationships (easily makes friends, struggles to keep them), family relationships (difficult), places where she is most comfortable (home), and least comfortable (school).
I asked her why school was hard, and she told me that people were always yelling at her, and that she worked really hard on her school work but no one noticed or appreciated it. I sent her for neuropsych testing for what I suspected was ADHD. I was as surprised as anyone when the testing came back. This B/C student in prestigious private schools had a full scale IQ of 80.
Christina illustrates the value of psychological testing in difficult cases. Once we had this key piece of information, the rest of her difficulties came into perspective, and we could begin to find solutions. I am likely to suspect learning disabilities when school is problematic, when kids complain that homework takes too much time, or when parents complain that homework time is a battle. “He’s not motivated,” or “she just doesn’t try,” are tip-offs.
Social kids like Christina are more likely to get missed. Children are intolerant of differences, so poor peer relations, including bullying and being bullied, may indicate a learning disability. Being great with adults or younger children but not so good with peers may also indicate trouble. Kids who won’t read for pleasure may have ADHD or dyslexia. Kids who don’t seem to understand you, or kids who answer a different question than you ask may be struggling with processing disorders.
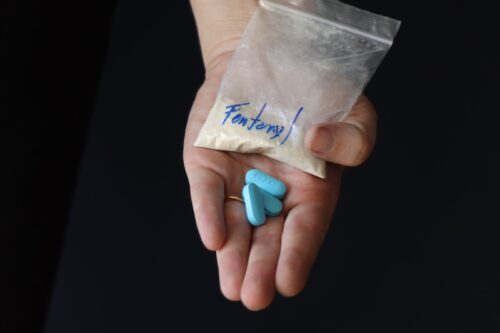
In addition to neuropsychological or educational testing, it is important to screen for other issues that may be causing the appearance of a learning disability. These might include hearing loss, visual impairments, trouble at home (chaos, abuse, or drug use, for example), or trouble at school (being bullied or rejected by peers, bullied by teachers, or having inappropriate academic demands—either too much or too little). Children with a history of a serious medical illness or a serious emotional trauma will drop off their developmental trajectories for a while because their energies have been spent coping rather than growing.
Absence seizure is another cause for apparent inattention or poor memory. If parents or teachers have reported staring spells, try hyperventilating the child in your office: Ask the child to count to 45 and to blow (hard) each time he or she says a number. An absence seizure can often be provoked this way and looks like a staring episode about 10 or 15 seconds long, often with lip smacking. More important, the child will stop counting, and will not respond to your gleefully shouting “elephants!” (Don’t say the child’s name—any child will ignore that.)
Interventions for learning disability need to focus on changing the child’s environment so that it’s working for her rather than against her. In Christina’s case, she was put in the local public school where she was given individual tutoring, extra time, and less demanding, but still mainstream, classes. She excelled, and the next time I saw her she said she loved her new school.
Family work is also crucial: Christina’s family needed to recalibrate their expectations for her, they needed to grieve their lost hopes for her, and they needed to forgive themselves for not realizing her needs before. They also needed practical knowledge about how Christina’s cognitive understanding of things translated into impulsivity and poor decision making, and needed strategies to help her rather than chastise her. Christina needed to repair her relationships with her siblings and her parents. In addition, she needed to stop seeing herself as lazy and bad.
While there is lots of therapy work to do, medications are not of much use in learning disabilities other than ADHD. Comorbid mental illness should be treated, of course. In global cognitive impairment, symptomatic treatment of impulsivity, lack of focus, or aggression can be necessary at times.
Understanding Patients with Severe Disabilities
When working with patients with more severe and global intellectual disabilities, the following are a few principles that have been helpful to me.
Examine the Time Course. Whether you are faced with the new evaluation of a child with intellectual disabilities or the review of someone known to you, be sure to get the actual time course of the behavior being considered. Twenty-nine days of minimal symptoms and one day of extremely frequent symptoms is not the same as thirty days of moderate symptoms. Bad mornings and good evenings usually say something about school demands, while good mornings and bad evenings may say something about the child’s ability to tolerate unstructured time. A lifetime of poor sleep may “merely” be the sequela of the structural brain differences that also cause the intellectual disability, whereas new onset of poor sleep probably indicates something else entirely.
Assess the Environment. Look for an environmental cause first. Children with intellectual disabilities generally don’t have the language facility to articulate their concerns, and they struggle with self-regulation even if they do. Therefore, behavioral symptoms quite frequently are the child’s attempt to express dislike. It is our job to figure out what they dislike and why. New staff or loss of favorite staff, new school peers or family members, even the change from summer and swimming to fall—and school—have been sources of behavioral symptoms.
Consider Medical Causes. At the same time, think of the medical causes. Aggression, compulsions, or self-injury may be signs of pain. Although I never made a proper study of it, I think the number one cause for admission to the Developmental Disabilities Unit where I was a resident was constipation. Think headache, sinuses, ears, teeth, throat, gastritis, constipation, diarrhea, appendicitis, and UTI, at least. Lactose intolerance is common and painful, too, while asthma is common and scary, particularly if the patient can’t explain what he is feeling.
Look at all of the Pieces of the Puzzle. Separate the child, the symptoms, and the jargon. Because so many of my patients with intellectual disabilities come with staff, counts, graphs, interpretations of the graphs and so on, it’s easy to lose sight of the usual constellations of symptoms. Short episodes of apparent intense fear is still likely to be panic in a child with intellectual disabilities. Likewise, having to touch the door frame every time they pass through it still suggests OCD. However, if you only get a graph of average crying episodes, tantrum duration, or self-injury, you may never realize that what precipitated the tantrum was intense fear or being prevented from touching the doorframe.
Medication and the Child with Cognitive Impairments
If you do choose to use medication, remember that we truly do not know what we are dealing with. We know for certain that the brain of a child with developmental disabilities is different from the average child’s brain, but we don’t know how it’s different. There could be more neurotransmitter receptors or fewer, the receptors could be more sensitive or less (or not functional at all), the connections could be in the “usual” pathways, or wired completely differently. Therefore, kids with mental retardation or autism may be more sensitive or less sensitive to medication, and there is no way of knowing ahead of time. I have patients who do well on 5 mg of fluoxetine dosed Mondays and Thursdays, and others who require 80 mg daily. Begin at a low dose and wait at least two weeks (and preferably much longer than that) between dosage changes.
An interesting study by John Rapp et al looked at behavioral sequelae of medication dose changes in a developmentally disabled population (Rapp et al, Behav Modification 2007;31(6):824–846). They found that irrespective of the change made—dose increases or decreases—behavior worsened the first week.
Making smaller changes over a longer time period can make for more successful tapers. Don’t let the immediate response to dose changes prevent you from tapering off medications that are no longer useful. I may take six months to taper a child off a medication, sometimes longer.
Just as we can’t be certain of the effects of any given medication, we also can’t be certain of the side effects of any medication. In my experience, children with intellectual impairments are more likely to have side effects and at least as likely to be upset by them as their normally developing peers.
My patient Ernie, a traumatized boy with an IQ of about 40, was very insistent that he wanted a new medicine, but couldn’t explain why. He pointed to himself repeatedly and said, “I want a new med.” When I asked why, he would point at himself again and say again, “I want a new med.” Finally, after asking him a lot of questions and getting the same answer, I finally got it. He wasn’t pointing to himself, he was pointing to his mouth. His antipsychotic was making him drool.
Child Psychiatry“My parents hate me,” she said. In reviewing her records, I saw that she’d tried just about every medication in the pharmacy, it seemed, with almost no effect. Because I was at a loss as to what else to do, I started over with diagnosis: mood (fine), anxiety (denies), sleep (fine), social relationships (easily makes friends, struggles to keep them), family relationships (difficult), places where she is most comfortable (home), and least comfortable (school).
I asked her why school was hard, and she told me that people were always yelling at her, and that she worked really hard on her school work but no one noticed or appreciated it. I sent her for neuropsych testing for what I suspected was ADHD. I was as surprised as anyone when the testing came back. This B/C student in prestigious private schools had a full scale IQ of 80.
Christina illustrates the value of psychological testing in difficult cases. Once we had this key piece of information, the rest of her difficulties came into perspective, and we could begin to find solutions. I am likely to suspect learning disabilities when school is problematic, when kids complain that homework takes too much time, or when parents complain that homework time is a battle. “He’s not motivated,” or “she just doesn’t try,” are tip-offs.
Social kids like Christina are more likely to get missed. Children are intolerant of differences, so poor peer relations, including bullying and being bullied, may indicate a learning disability. Being great with adults or younger children but not so good with peers may also indicate trouble. Kids who won’t read for pleasure may have ADHD or dyslexia. Kids who don’t seem to understand you, or kids who answer a different question than you ask may be struggling with processing disorders.
In addition to neuropsychological or educational testing, it is important to screen for other issues that may be causing the appearance of a learning disability. These might include hearing loss, visual impairments, trouble at home (chaos, abuse, or drug use, for example), or trouble at school (being bullied or rejected by peers, bullied by teachers, or having inappropriate academic demands—either too much or too little). Children with a history of a serious medical illness or a serious emotional trauma will drop off their developmental trajectories for a while because their energies have been spent coping rather than growing.
Absence seizure is another cause for apparent inattention or poor memory. If parents or teachers have reported staring spells, try hyperventilating the child in your office: Ask the child to count to 45 and to blow (hard) each time he or she says a number. An absence seizure can often be provoked this way and looks like a staring episode about 10 or 15 seconds long, often with lip smacking. More important, the child will stop counting, and will not respond to your gleefully shouting “elephants!” (Don’t say the child’s name—any child will ignore that.)
Interventions for learning disability need to focus on changing the child’s environment so that it’s working for her rather than against her. In Christina’s case, she was put in the local public school where she was given individual tutoring, extra time, and less demanding, but still mainstream, classes. She excelled, and the next time I saw her she said she loved her new school.
Family work is also crucial: Christina’s family needed to recalibrate their expectations for her, they needed to grieve their lost hopes for her, and they needed to forgive themselves for not realizing her needs before. They also needed practical knowledge about how Christina’s cognitive understanding of things translated into impulsivity and poor decision making, and needed strategies to help her rather than chastise her. Christina needed to repair her relationships with her siblings and her parents. In addition, she needed to stop seeing herself as lazy and bad.
While there is lots of therapy work to do, medications are not of much use in learning disabilities other than ADHD. Comorbid mental illness should be treated, of course. In global cognitive impairment, symptomatic treatment of impulsivity, lack of focus, or aggression can be necessary at times.
Understanding Patients with Severe Disabilities
When working with patients with more severe and global intellectual disabilities, the following are a few principles that have been helpful to me.
Examine the Time Course. Whether you are faced with the new evaluation of a child with intellectual disabilities or the review of someone known to you, be sure to get the actual time course of the behavior being considered. Twenty-nine days of minimal symptoms and one day of extremely frequent symptoms is not the same as thirty days of moderate symptoms. Bad mornings and good evenings usually say something about school demands, while good mornings and bad evenings may say something about the child’s ability to tolerate unstructured time. A lifetime of poor sleep may “merely” be the sequela of the structural brain differences that also cause the intellectual disability, whereas new onset of poor sleep probably indicates something else entirely.
Assess the Environment. Look for an environmental cause first. Children with intellectual disabilities generally don’t have the language facility to articulate their concerns, and they struggle with self-regulation even if they do. Therefore, behavioral symptoms quite frequently are the child’s attempt to express dislike. It is our job to figure out what they dislike and why. New staff or loss of favorite staff, new school peers or family members, even the change from summer and swimming to fall—and school—have been sources of behavioral symptoms.
Consider Medical Causes. At the same time, think of the medical causes. Aggression, compulsions, or self-injury may be signs of pain. Although I never made a proper study of it, I think the number one cause for admission to the Developmental Disabilities Unit where I was a resident was constipation. Think headache, sinuses, ears, teeth, throat, gastritis, constipation, diarrhea, appendicitis, and UTI, at least. Lactose intolerance is common and painful, too, while asthma is common and scary, particularly if the patient can’t explain what he is feeling.
Look at all of the Pieces of the Puzzle. Separate the child, the symptoms, and the jargon. Because so many of my patients with intellectual disabilities come with staff, counts, graphs, interpretations of the graphs and so on, it’s easy to lose sight of the usual constellations of symptoms. Short episodes of apparent intense fear is still likely to be panic in a child with intellectual disabilities. Likewise, having to touch the door frame every time they pass through it still suggests OCD. However, if you only get a graph of average crying episodes, tantrum duration, or self-injury, you may never realize that what precipitated the tantrum was intense fear or being prevented from touching the doorframe.
Medication and the Child with Cognitive Impairments
If you do choose to use medication, remember that we truly do not know what we are dealing with. We know for certain that the brain of a child with developmental disabilities is different from the average child’s brain, but we don’t know how it’s different. There could be more neurotransmitter receptors or fewer, the receptors could be more sensitive or less (or not functional at all), the connections could be in the “usual” pathways, or wired completely differently. Therefore, kids with mental retardation or autism may be more sensitive or less sensitive to medication, and there is no way of knowing ahead of time. I have patients who do well on 5 mg of fluoxetine dosed Mondays and Thursdays, and others who require 80 mg daily. Begin at a low dose and wait at least two weeks (and preferably much longer than that) between dosage changes.
An interesting study by John Rapp et al looked at behavioral sequelae of medication dose changes in a developmentally disabled population (Rapp et al, Behav Modification 2007;31(6):824–846). They found that irrespective of the change made—dose increases or decreases—behavior worsened the first week.
Making smaller changes over a longer time period can make for more successful tapers. Don’t let the immediate response to dose changes prevent you from tapering off medications that are no longer useful. I may take six months to taper a child off a medication, sometimes longer.
Just as we can’t be certain of the effects of any given medication, we also can’t be certain of the side effects of any medication. In my experience, children with intellectual impairments are more likely to have side effects and at least as likely to be upset by them as their normally developing peers.
My patient Ernie, a traumatized boy with an IQ of about 40, was very insistent that he wanted a new medicine, but couldn’t explain why. He pointed to himself repeatedly and said, “I want a new med.” When I asked why, he would point at himself again and say again, “I want a new med.” Finally, after asking him a lot of questions and getting the same answer, I finally got it. He wasn’t pointing to himself, he was pointing to his mouth. His antipsychotic was making him drool.
KEYWORDS child-psychiatry
Issue Date: October 1, 2010
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)