Dosing is not a collaborative venture when it comes to controlled substances, and here we look for the safe upper limits of stimulant dosing.
Publication Date: 02/19/2024
Duration: 22 minutes, 23 seconds
Transcript:
KELLIE NEWSOME: How high can you go? Today, we look at the upper limits of stimulant dosing.
CHRIS AIKEN: Welcome to the Carlat Psychiatry Podcast, keeping psychiatry honest since 2003. I’m Chris Aiken, the editor in chief of the Carlat Report.
KELLIE NEWSOME: And I’m Kellie Newsome, a psychiatric NP and a dedicated reader of every issue. We’re continuing our countdown of the most-read articles from 2023 with #3 on the list, Stimulant Dosing Limits, by Kelvin Quiñones-Laracuente, MD, PhD and Chris Aiken, MD. You can read all of the top 15 articles free online through the link in the show notes or just Google “Top 15 Carlat Psychiatry Articles of 2023.” Dr. Quiñones-Laracuente is an Assistant Professor, Department of Psychiatry at NYU Grossman School of Medicine, and he wrote this piece in his final year of residency at NYU where Dr. Aiken taught a course on medical writing. He and Dr. Aiken have no disclosures related to this material.
CHRIS AIKEN: No disclosures, but the piece was inspired by a patient scenario that comes up with increasing frequency. We’re seeing more and more adults patients come in on high-dose stimulants. The floodgates opened up in 2004 when stimulants first got approved for adult ADHD, a diagnosis that brings together two unfortunate forces in medicine. On the one hand, the treatment is a highly rewarding, sought after substance that has a long history of overuse in the US. On the other hand, the diagnosis is difficult to make – requiring a childhood history which is nearly impossible to pin down in adults, and symptoms that show up in most other psych disorders or in normal people who are stressed or sleep deprived. I don’t have any research to back this up, but my guess is that when stimulants are used to treat real ADHD people respond well and keep responding well – they don’t need dose escalation. But when they are used off label they have imperfect effects. They improve some areas of cognition, but worsen others, and there initial benefits tend to wear off, causing patients to ask for higher and higher doses.
KELLIE NEWSOME: Let’s get into the article, and I understand you have an update for us at the end.
CHRIS AIKEN: Yes I’m very excited about this update. This was a hard piece to write, because there were no good reviews that focused on stimulant dosing, so we had to search through all the studies to see which doses were used. We did our best on a low budget. But a few months after we published it the piece we were looking for came out – a scientific review of high-dose stimulants in JAMA Psych.
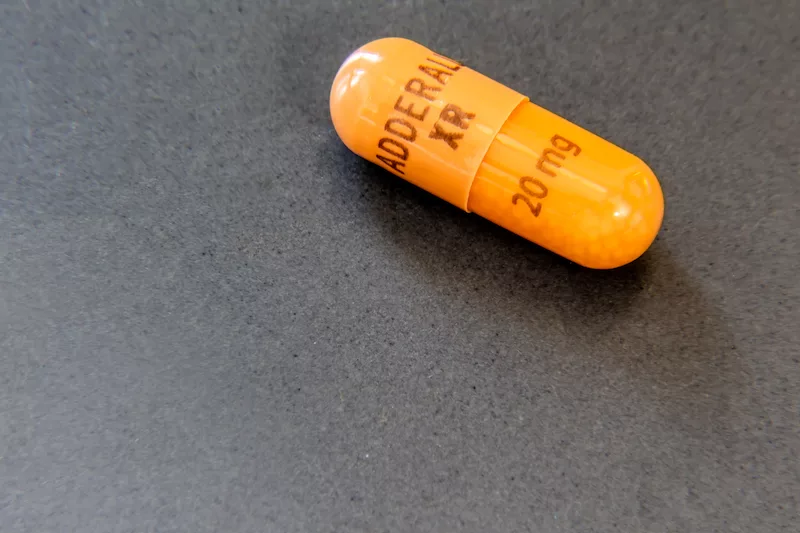
KELLIE NEWSOME: We’ll get to that later. Let’s start with a case. “Amanda” is an engineering student with ADHD. After six years of treatment, she says her current dose of Adderall XR (40 mg) does not work like it used to. You note that 40 mg daily is the listed FDA maximum daily dosage of Adderall, and you are unsure whether to increase the dose or not.
CHRIS AIKEN: If this were a case of depression, we might just raise the dose a little, even if we’re only hoping for a placebo effect in the untested range. But stimulants are different. These medications are inherently rewarding, which means we can’t take a purely collaborative approach and let patients guide the dose. But how high can we go? That isn’t as clear as we’d like. Even though they are tightly controlled as Schedule II drugs, the FDA is not always clear about what the max dose is.
KELLIE NEWSOME: So what could go wrong in going higher? A higher dose raises the risk of abuse and diversion, as well as cardiovascular problems like hypertension, stroke, and myocardial infarction. It may even worsen cognition, either by disrupting sleep or causing a hyperfocused state that makes it difficult for the patient to shift gears and change tasks. And then there’s psychiatric problems – psychosis and mania become more likely as the dose inches up. When patients with narcolepsy took high doses of stimulants (approximately double the FDA maximum), it raised their risk of psychosis (12-fold), psychiatric hospitalization (three-fold), and substance abuse (four-fold), according to a study that compared outcomes in high and low doses (Auger RR et al, Sleep 2005;28(6):667–672).
CHRIS AIKEN: That’s a remarkable study because it was done in narcolepsy, so those patients didn’t necessarily have psychiatric disorders to begin with. I worry that the consequences would be worse in a psychiatric population.
KELLIE NEWSOME: We don’t often talk about animal studies, but in an area like this that is largely untested in humans the animal data is informative, and they don’t look good for high dose stimulants,
particularly the amphetamines. Studies with baboons have shown damage in striatal dopaminergic terminals on elevated doses of amphetamines, equivalent to 60 mg/day and above in human dosing (Ricaurte GA et al, J Pharmacol Exp Ther 2005;315(1):91–98). At higher doses, animal studies reveal neurotoxic damage to dopaminergic neurons in the caudate putamen (Moratalla R et al, Prog Neurobiol 2017;155:149–170).
Now let’s look at the what we know about doing, starting with the amphetamines, but first a preview of the CME quiz for this episode. Find a link to the full quiz in the show notes or on the podcast page of the Carlat Report website.
1. For which disorder does the FDA allow dosing of mixed amphetamine salts (Adderall) up to 60 mg per day?
A. ADHD
B. Narcolepsy
C. Adult ADHD
D. ADHD with CYP2D6 rapid metabolism
CHRIS AIKEN: The FDA sets the maximum for Adderall (IR or XR) at a dose of 40 mg/day for adult ADHD. However, they allow up to 60 mg/day for more severe cases of ADHD, as well as for narcolepsy. That 40–60 mg max was derived from a large registration trial of adult ADHD. The study compared three doses of Adderall XR (20, 40, and 60 mg/day), and found no significant difference between them in terms of safety and efficacy (Weisler RH et al, CNS Spectr 2006;11(8):625–639). There was some evidence that people with more severe ADHD did better on the higher doses of 40–60 mg, but that finding was limited due to its secondary, “data-fishing” nature.
We recommend thinking of the dose in three zones: the safe zone (below 40 mg/day), the gray zone (40–60 mg/day), and the danger zone (above 60 mg/day). Going up to 60 mg/day may be justified when the symptoms are severe, but you’d want to document their presence on the mental status exam and verify that the ADHD is affecting the patient’s functioning. We are not aware of research justifying a dose above 60 mg/day, which would land in the danger zone.
Higher doses may also be justified when a longer duration is needed. Mydayis (a very extended-release version of Adderall) has a maximum dose of 50 mg, but this leads to similar plasma levels as Adderall XR 40 mg because the dose is spread out over 16 hours instead of 12. When extending the duration, make sure the patient is getting adequate sleep so they are not relying on the stimulant for symptoms of sleep deprivation.
KELLIE NEWSOME: For methylphenidates like Ritalin and Concerta, the FDA gives a clear maximum, although it varies slightly by formulation. That max is 60 mg/day for methylphenidate instant release, but higher doses are allowed for products with longer durations such as Concerta (72 mg over 12 hours) and Adhansia (100 mg over 16 hours).
A few methylphenidate products have lower dose caps because more of the drug is absorbed. These include the transdermal formulation (Daytrana is given at half the usual methylphenidate dose) and orally disintegrating tablets (Cotempla ODT is dosed at 86% of the usual dose and Adzenys ODT at 65%).
So the FDA is vague about the safe upper limits of amphetamines, placing it around 40-60 mg for Adderall, but they are pretty clear about the upper limits with methylphenidate. You’ll need to check in the prescribing information as it varies for each methylphenidate formulation, or you can view the table in the online Carlat article. One caveat: We’re talking about adult dosages here, things may be a little different in children, but Dr. Aiken what about in the elderly?
CHRIS AIKEN: Adult ADHD is a relatively new concept, and geriatric ADHD is newer still. The middle-aged patients who started stimulants 20 years ago—when the FDA first approved them in adults—are now entering their retirement years with little data to guide them. There are no controlled trials in patients with ADHD after age 50, but a few observational studies suggest older adults continue to benefit, although at lower doses (eg, average doses of 30 mg/day for methylphenidate and 10 mg/day for amphetamine and dextroamphetamine) (Michielsen M et al, J Atten Disord 2021;25(12):1712–1719).
There are three reasons to consider lowering the dose as patients age. Older adults are more susceptible to the cardiovascular effects and—based on animal data—the neurotoxic effects of stimulants. In animal models, the same dose of amphetamine reached twice the levels in the brains of older rats compared to younger ones, suggesting that older adults may not need as high a dose to achieve a good response (Berman SM et al, Mol Psychiatry 2009;14(2):123–142).
KELLIE NEWSOME: But what about patients who are rapid metabolizers or have drug interactions that might lower the stimulants? I remember a patient who came to see me on 180 mg/day of methylphenidate, she said her psychiatrist had told her she needed a high dose because she metabolizes the stimulant quickly.
CHRIS AIKEN: Stimulant metabolism is complex, so I wouldn’t jump to that conclusion based on genetic testing or drug interactions alone. If you do suspect an interaction like that, you can test for serum levels of amphetamines or methylphenidate first to see if they are low. But most drug interactions are inhibitors – raising drug levels – not inducers which lower the levels. The amphetamines are a major substrate of CYP2D6, so strong CYP2D6 inhibitors (which include bupropion, duloxetine, fluoxetine, and paroxetine) may push the dose even higher. In terms of food, most stimulants are not significantly affected by food interactions, but Adderall XR may not be absorbed as well when taken with a large, fatty meal.
KELLIE NEWSOME: Back to Amanda’s case. Going beyond 40 mg/day of Adderall would land us in the gray zone for this student. Before taking that step, we should verify that her ADHD is causing significant functional impairment and rule out other causes such as sleep deprivation or depression. Besides raising the dose, evidence also supports augmenting with guanfacine or switching to a different amphetamine mixture (eg, dextroamphetamine, lisdexamfetamine). If—after discussing risks and benefits—we decide to raise the dose, we should track her progress with a rating like the Adult ADHD Self-Report Scale.
The bottom line: With psychostimulants, it’s best to stay within the FDA-approved limits. Slightly higher doses of mixed amphet- amine salts (Adderall, up to 60 mg/day) may be needed for patients with severe symptoms, and lower doses are likely safer and just as effective in the elderly.
Or at least, that’s the bottom line we ended with. What did you learn from the research update?
CHRIS AIKEN: Yes this study comes to us from Luis C. Farhat, MD from Sao Paula, Brazil, and the research team includes some top meta-analytic minds like Andrea Cipriani, Toshi Furukawa, and Samuele Cortese. They pulled together 47 randomized controlled trials in adult ADHD and created dose response curves for methylphenidate and amphetamines to see whether their efficacy – and their risk of side effects and drop-outs – changed as the dose rose above the FDA limits. To even things out across formulations they converted to instant release methylphenidate or Adderall dose equivalents, and they interpreted the FDA max as 60 mg/day for methylphenidate or 40 mg/day for Adderall.
I wish I could show you the curves, but I’ll post them on my social media feeds today – Monday. Here’s what you’ll see. For methylphenidate, there is steady improvement beyond 60mg/day, up to 85mg/day, but it comes at a cost. The adverse effects also start to rise after the FDA max of 60mg/day. For amphetamines, we don’t see much benefit after about 35mg/day, which is below the FDA max of 40mg/day, and after about 45-50mg/day the line tips the other way – the ADHD symptoms seem to worsen, though not in any statistically significant kind of way. As with methylphenidate, the risk of adverse effects rises steady with the dose, and the studies tested up to 75mg/day of Adderall equivalents.
KELLIE NEWSOME: In the methylphenidate analysis they went up to 85mg/day, and some of the improvement they saw there may be due to the Adhansia studies where the dose is stretched out throughout the day. Adhansia XR is the longest lasting methylphenidate – clocking in at around 16 hours. It’s generally approved up to 85mg/day, although the pdr mentioned they went up to 100mg/day in the studies but saw more side effects at that point. So what I’m saying is that how high you go ought to depend on the duration of the drug – if the patient is getting 16 hours coverage they’ll need more daily dosage than 8 hours coverage.
CHRIS AIKEN: Yes I agree, and my own experience is also in line with this paper. I tend to see more psychiatric problems on high dose amphetamines than I do on high dose methylphenidate – we have a webinar on that issue on the Carlat Website called Amphetamine vs Methylphenidate if you’d like to learn more.
But Kellie you asked if I had any disclosures and I should add this one: I am an adult psychiatrist, and the research we discussed in this episode is from adult studies. I asked our child editor Josh Feder how he’d apply it to children. He said dosing varies a lot from person to person, and sometimes they need to go beyond the max. He also reminded us of something that applies to adults as well – all this research is based on averages, and there are always outliers in those averages. I agree. The challenge is that you need to look at functioning – and get objective or 3rd party reports on that like grades or job performance or task completion. Don’t just take the patient’s word for it. There ADHD may be well controlled, but sleep deprivation, temporary stress, depression, or the rewarding qualities or even medication misuse or sharing meds may be prompting requests for higher doses.
KELLIE NEWSOME: Check out the online article which has a Carlat table of dose ranges for the stimulant formulations. Join us next week for #2 in the top articles: Deprescribing Anti-anxiety Medications in Older Adults. Meanwhile, get daily research updates on Dr. Aiken’s social media feeds – search for ChrisAikenMD on twitter, linkedin, facebook, and that new one – Threads. Thank you for making us the #1 downloaded psychiatry podcast in 2023.
__________
The Carlat CME Institute is accredited by the ACCME to provide continuing medical education for physicians. Carlat CME Institute maintains responsibility for this program and its content. Carlat CME Institute designates this enduring material educational activity for a maximum of one quarter (.25) AMA PRA Category 1 CreditsTM. Physicians or psychologists should claim credit commensurate only with the extent of their participation in the activity.

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



