DSM-5 has adopted many of the concepts from Hagop Akiskal’s Bipolar Spectrum, but not in the way he had planned. Here we trace his thinking back to the early 1970’s, when Dr. Akiskal reshaped the way we think about depression by blurring the boundary between stress-induced and biological depression.
Published On: 3/15/2021
Duration: 26 minutes, 19 seconds
Rough Transcript:
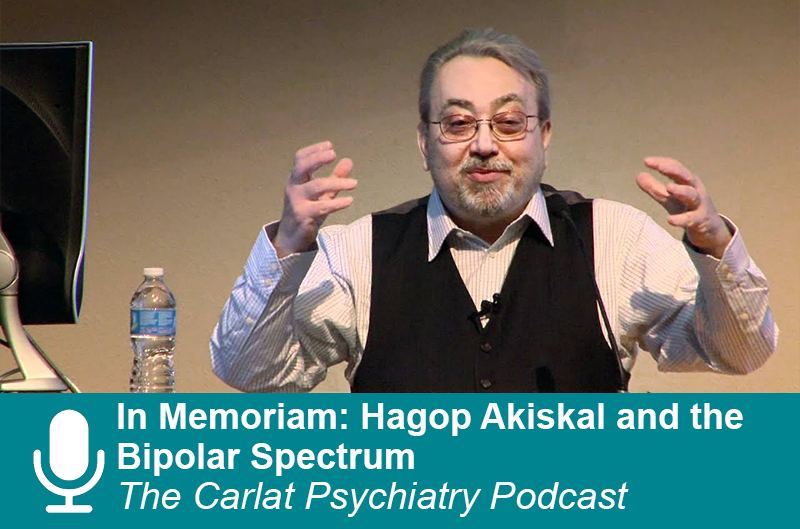
Hagop Akiskal was known for the bipolar spectrum, but that was just the latest in a 50 year career that constantly pushed psychiatry in new directions. He lived on the cutting edge. As soon as his ideas entered the mainstream, he moved on to the next controversy, and on January 20th 2021 he moved on from this life. Today, we look back on his legacy.
Welcome to the Carlat Psychiatry Podcast, keeping psychiatry honest since 2003. I’m Chris Aiken, the editor in chief of the Carlat Report. And I’m Kellie Newsome, a psychiatric NP and a dedicated reader of every issue.
It’s rare for a scientific paper to fetch much on the black market, but Hagop Akiskal was no ordinary psychiatrist.
[Hagop Akiskal]
And that monograph he’s talking about is currently selling for $700-900 on Amazon. It was an issue of the Psychiatric Clinics of North America that Hagop guest edited in 1999, and a paper he authored in that issue became one of his most influential – and controversial. In it he laid out a spectrum of bipolar disorders from the most manic-psychotic extreme – schizoaffective disorder – to cases of bipolar that are only unleashed by substance abuse, antidepressants, or brain atrophy from dementia…
[Hagop]
All but two of those categories have been absorbed into the DSM, which now includes:
Bipolar I
Bipolar II
Cyclothymic disorder (which Hagop views as the temperamental underpinnings of borderline personality disorder and calls Bipolar II ½ when it occurs with the longer depressions of bipolar II)
Bipolar III – antidepressant induced mania is now categorized as bipolar in DSM-5 – largely based on the research of Hagop and others who showed that over 90% of patients with antidepressant induced mania go on to develop full bipolar disorder with long term follow up.
Bipolar IV – hyperthymic temperament with depression – OK this one didn’t make it into the DSM
Bipolar IV and ½: Substance induced bipolar disorder
Bipolar V: Depression with mixed features
Bipolar VI: Mania in the context of dementia. Hagop believed that the brain atrophy of dementia could unleash a latent bipolar disorder in people with genetic or other risks for bipolar, but this category is not recognized in DSM unless you count it as bipolar due to a general medical condition.
Kellie Newsome: And yet, you can hear in that quote that Hagop is not satisfied – he’s looking for a fight – he says his conceptualization was done in defiance of DSM, “even the current DSM.”
Dr. Aiken: Hagop was a passionate man who wore his heart on his sleeve. I spent a few days with him in 2010 when he visited North Carolina for a conference and remember him a warm man who was keenly interested in the people around him. He was a poet, a romantic, and a scientist who thrived on controversy. Here he is in 2012, giving a grand rounds where some of the committee members of DSM-5 were in attendance. He called out those committee members in the middle of the lecture – even though they had absorbed many of the changes he had pushed for, he called on them for more.
[Hagop quote[
Kellie Newsome: What more did he want?
Dr. Aiken: He believe the cut-off duration for hypomania should be shorter than 4 days. You could argue that the data was on his side. There are a lot of patients with short-duration hypomania, and they have similar treatment responses and family histories as those with full bipolar II. In fact, even for patients with true DSM-5 bipolar II, most of their hypomanias only last 2-3 days, so you could easily miss many of them when you ask about the duration. DSM-5 did recognize this category, but it’s in the experimental section in the back of the book.
The Bipolar Spectrum
Kellie Newsome: Hagop’s work on the bipolar spectrum garnered controversy, but he wasn’t trying to bring something new to psychiatry. He was trying to bring it back to the way it was in Kraeplin’s time. Emil Kraeplin was the first psychiatrist to fully lay out the modern description of manic-depression, and when he used that word he meant patients with just mania, just depression, or both. Kraeplin spent years trying to tease apart the manic or bipolar end from the depressive patients, but he eventually concluded – in his words - “this classification, apparently so simple, really encounters manifold difficulties.” One reason he could not separate them was mixed states – where depression and mania overlap. When he looked closely, he saw these mixed states in depressed patients who never went into mania. Today, DSM-5 recognizes that mixed states can occur in non-bipolar patients, and classifies them as major depression with mixed features – which affects up to 25% of people with recurrent depression.
[Hagop quote]
Dr. Aiken: Hagop first started writing about the bipolar spectrum in the early 1980s, along with other psychiatrists who took up the mantle like Jules Angst – the Swiss psychiatrist who first proposed the separation of mood disorders into bipolar and unipolar in the 1960’s. By the time DSM-III made that separation official in 1980, Dr. Angst had moved in other directions. Like Kraeplin and Akiskal, he too was dissatisfied with the rigid lines in the DSM. Angst believed that bipolar could be understood as both a categorical illness – with a clean separation between bipolar and unipolar - and a spectrum – with a smooth continuum between the two. He often compared it to blood pressure – which rises continuously from normal to high, but at some point reaches an arbitrary cut-off that we call hypertension. But before we get more into the bipolar spectrum, let’s go back to Hagop’s early career. He started a revolution back then as well – one that we now take for granted because it has become so widely absorbed into the way we think about depression.

Hagop Akiskal: A Brief Sketch
Kellie Newsome: Hagop was Armenian, but was born in the capital city of Lebanon – Beruit. His parents were artists and scientists, and his family was scarred by the legacy of genocide which left a mark on Hagop
[Hagop]
He came to America in 1969 to complete his psychiatric residency at the University of Wisconsin in Madison. There he worked with William McKinney on animal models of depression. And at the end of his residency he published a paper with McKinney in the journal Science that would change how we think about depression. The 1973 article was called Depressive disorders: toward a unified hypothesis, and his intent was not to unify bipolar and unipolar.
Dr. Aiken: At the time, DSM lumped mania and depression together in one illness, and in this article Hagop actually gave 5 reasons why he thought they were separate conditions.
Kellie Newsome: He may be the only psychiatrist who actively fought to change DSM II, III, IV, and 5.
Dr. Aiken: In this paper Hagop sought to unify all the theories of depression that existed at the time, and to integrate them into a biological framework. At the time, DSM II split depression into two types – there was the psychological type “exogenous depression” which was due to outside stressors and was thought best treated with psychotherapy. Then there was the biological type “endogenous depression” which was thought due to biological or genetic factors and treated with medications. Using neuroscience and animal models, Hagop showed that even stress-induced depressions had a biological basis. He cited research that so-called endogenous depression was just as likely to be triggered by stress as the other type, and gave this clinical pearl: Patients with severe, endogenous depression were often so cognitively blunted that they were unable to recall the stress that precipitated their episode, giving psychiatrists the false impression that it came on out of nowhere. In his view, the psychoanalytic view of depression – that it was a mourning for lost relationships – was entirely consistent with the biological literature on attachment in animals, and the behavioral theory was validated by the research on learned helplessness. He argued that these schools of thought spoke different languages but had compatible ideas and should adopt a more integrated theory that could lead to better research – and that is what DSM-III did with major depressive disorder.
Cyclothymic Disorder
Kellie Newsome: Getting back to the bipolar spectrum. After his paper in Science, Hagop laid low and didn’t publish much. He moved to the University of Tennessee in Memphis, where he opened one of the first mood clinics in America. People started referring patients to him who did not have classic bipolar but had some bipolar features, and he recognized in many of them a temperament that Emil Kraeplin had written about: Cyclothymia.
[Hagop quote]
Dr. Aiken: Hagop followed these cyclothymic patients for 3 years and compared them to a group with personality disorders and another group with bipolar disorder. In 1977 he published his 2nd major paper, which showed that the cyclothymic patients were more like the bipolar patients than the ones with personality disorders. They resembled bipolar patients in their family history, treatment response – nearly half developed mania on tricyclics - and their course of illness - about a third went on to develop full bipolar disorder. Based on this study, the DSM committee included cyclothymia in the new edition, but not in the way that Hagop intended.
Kellie Newsome: There are at least 2 differences. First, in the DSM, you cannot diagnose cyclothymic disorder if the patient also has another bipolar disorder, like Bipolar I or II. But Hagop saw temperaments like cyclothymia as overlapping with mood disorders, and changing the way those mood episodes came out, much as a picture looks different when it’s printed on yellow paper instead of white. In the case of cyclothymia, he was particularly interested in how it overlapped with bipolar II disorder – he called this overlap bipolar II ½ and wrote that these patients had a stormier course that often resembled borderline personality disorder. He may have been on to something. He found that 38% of bipolar II’s had cyclothymic temperament, and a recent meta-analysis concluded that 38% of bipolar II’s have borderline personality disorder…now, that doesn’t prove anything, but it’s quite possible these 38% are the same patients, just called by different names – cyclothymia with bipolar II, and borderline personality with bipolar II.
Dr. Aiken: Marsha Linehan seems to agree with Hagop’s conceptualization, though she didn’t reference him directly. In her textbook on dialectical behavioral therapy, she wrote that patients with borderline personality disorder had a unique temperament – an inborn difference – that was more labile and aggressive. She said that “cycloid personality” was “in many ways similar to my own view” of this temperament.
Kellie Newsome: Cycloid personality was actually the working title for borderline personality disorder in the early drafts of DSM III, and it reads a lot like Hagop’s description of cyclothymia. “Irregular energy levels” with “intense, variable moods,” where depression predominates but is interspersed by brief periods of “elation . . . dejection, anxiety, or impulsive anger.”
Dr. Aiken: The other thing that Hagop thought DSM got wrong about cyclothymic disorder was – he didn’t think it was a disorder. Hagop had a deep respect for temperament, he wrote that the psychiatrist should help the patient bring out what is best in their temperament instead of over-medicating it with aggressive pharmacology. Temperament – in his view – was the bridge between madness and genius. People with affective temperaments can change the world in creative ways, if we help them bring out the best in their unique dispositions.
[Hagop]
Kellie Newsome: Hagop described 5 affective temperaments that were more common in people with mood disorders – and more common in their relatives. He created the TEMPS-A rating scale to identify them. They are:
- Dysthymic
- Hyperthymic
- Cyclothymic
- Anxious
- Irritable
Around 50% of people with bipolar disorder have one of these temperaments, and these traits are more common in the relatives of people with mood disorders. You can find the scale at www.psychiatryletter.net under the Resources tab. Cyclothymic and dysthymic temperaments made it into the DSM, although dysthymic was later merged into the broader category of chronic depressive disorder.
Dr. Aiken: When he was asked in 2008 about what he was most proud of in his career, Hagop cited his work on dysthymic disorder. This low-grade depression was thought of as a personality disorder that bore only a superficial resemblance to major depression, but Hagop showed that when you put a dysthymic patient in the sleep lab you see a distinct feature that is biological marker of major depression: the REM phase comes on faster – called REM latency.
[Hagop]
Dr. Aiken: And I can see that smile on his face. Hagop loved to incite controversy, but in his heart he was a unifier. He wanted to break down the boundaries between exogenous and endogenous depression, between bipolar and unipolar depression, and – ultimately – between mental illness and normality.
Kellie Newsome: How so?
Dr. Aiken: In part, that was what his temperament model was about – that the reason mood disorders persist is that the genes that cause them are associated with character strengths – and those genes persist in many of us who don’t have mood disorders ourselves. Hagop helped break down the “us and them” mentality between doctor and patient. He told me once that in the old days the psychiatrist lived on the hospital grounds and got to know what the lives of their patients were really like – day and night. He thought we had lost touch with that – and only saw them through the abstract lens of the DSM and the 15 minute medication visit. But, you know, a lot of us in the field have close friends or family who’ve had mental illness or have had personal experience with it ourselves. Sure, there are boundaries that need to be preserved there, and I don’t advocate treating your friends and relatives, but I think all psychiatrists should have a good friend with bipolar disorder, schizophrenia, autism, substance abuse or something. It helps us remember that patients are more like us than not, and that the problems they come to us for help with affect them in ways far deeper than an eight item rating scale.
Hyperbolic Taper
And now for the word of the day…. Hyperbolic taper
When you taper off an SSRI or a benzo, you can lower the dose linearly, such as 20mg/day for a week, 10mg for a week, 5mg / day for a week then stop. But the medication does not disengage from the receptor in a linear fashion. To account for this and prevent withdrawal problems, Drs. Horowitz and Taylor developed the hyperbolic taper. It’s similar to the “long tail” taper that is used with benzodiazepines. You go down quickly at first and then taper off by increasingly small amounts towards the end. The idea is to for the occupancy at the serotonin receptor to drop by 10% with each dose reduction. The exact milligrams at each step vary for each antidepressant, and we have a guide online in our June 2019 issue. In next weeks podcast, we’ll delve into this and more in an interview with Swapnil Gupta on How to Stop Antidepressants, Benzos, and Stimulants.
We’d like to thank the University of New Mexico and the American College of Neuropsychopharmacology for the audio of Hagop Akiskal, which was recorded in 2008 and 2012. And special thanks to David Aiken for some of the music in this episode.
Got feedback? Take the podcast survey.

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)



