Clozapine: Monitoring With Skill
You probably know that clozapine is FDA approved for treatment-resistant schizophrenia, defined as the failure of two or more antipsychotic medications prescribed with adequate dosing and treatment duration. It has an additional FDA-approved indication that is less well known: suicidal behavior in patients with schizophrenia or schizoaffective disorder. For both indications, clozapine is one of the best antipsychotics in our arsenal. However, it comes with significant potential side effects that require strict monitoring and careful dosing. Below, I review current guidelines for prescribing clozapine and monitoring for side effects.
'Clozapine initiation and dosing
'First, you will need to become certified in the Clozapine REMS program at www.newclozapinerems.com/Public/home/Prescriber. Enroll your patient at the same website and include their baseline absolute neutrophil count (ANC). A patient’s ANC must be at least 1500/µL, unless they have benign ethnic neutropenia (see box) in which case the ANC should be at least 1000/µL and checked twice. Once your patient is enrolled, you’ll need to submit the ANC as part of the monthly patient status form.
Since clozapine increases the risk of metabolic syndrome, I also obtain a baseline metabolic panel (including fasting blood glucose), weight, lipid panel, blood pressure measurement, physical exam with heart disease risk assessment, and ECG. ECG is particularly important for patients with a history of or risk for cardiovascular disease. Clozapine is prolactin-sparing, so I don’t normally obtain baseline prolactin levels unless I am switching from a non-prolactin-sparing medication and want to make sure prolactin levels normalize after the switch.
Starting low and going slow is crucial to minimize adverse effects from clozapine. Start with 12.5 mg once or twice per day and increase by 25–50 mg per day until you reach a minimum therapeutic dosage of 250–450 mg by the end of two weeks. From there, you can increase one or two times per week by up to 100 mg at a time. The maximum daily dose is 900 mg.
It’s not unusual for patients to miss occasional clozapine doses, but if they miss their doses for two days or longer, reduce the dose to 12.5 mg once or twice per day and reinitiate the titration. You can increase the dose faster than previously (eg, by 50 mg per day rather than 25 mg), but keep in mind there are no specific guidelines about this faster titration. 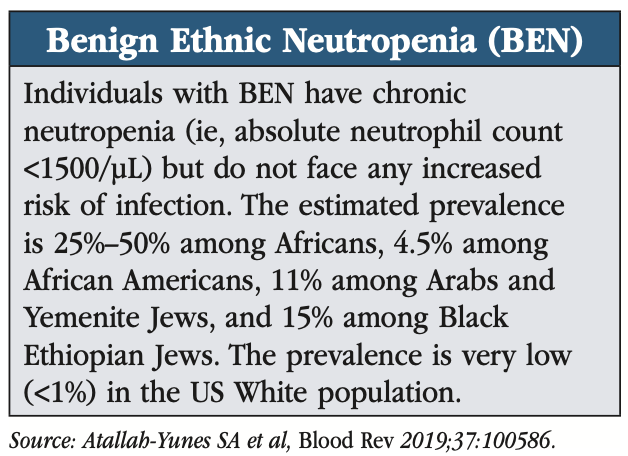
Therapeutic drug monitoring
Check a clozapine plasma level after five to seven days on the initial target dose by obtaining a trough level 10–12 hours after the last dose. The therapeutic range is 350–600/µL (Correll CU et al, CNS Drugs 2022;36(7):659–679). If the plasma level is higher than 600/µL, the risk of seizures increases; consider adding an anticonvulsant like sodium valproate (Depakote) if this higher plasma level is required to manage the patient’s symptoms.
Plasma levels tend to be lower in males, younger patients, those using CYP450 inducers (eg, some anticonvulsants), and patients who smoke tobacco or cannabis. Levels tend to be higher in Asian patients, caffeine users, patients on CYP450 inhibitors (eg, oral contraceptives, fluvoxamine, some antifungals and antibiotics), and patients with infectious illnesses (Correll et al, 2022).
Some sources recommend checking clozapine blood levels as necessary or every three months if the dose is 600 mg or higher. I prefer ongoing measurements of clozapine blood levels every three to six months regardless of dose, especially because fluctuating levels in patients with schizophrenia are predictive of relapses leading to hospitalization (Hiemke C et al, Pharmacopsychiatry 2018;51(01/02):9–62). Check more frequently if the patient:
- Has difficulties with medication adherence
- Has an exacerbation of side effects
- Becomes or remains symptomatic
- Changes their tobacco/cannabis smoking status
- Begins a new drug that may affect clozapine blood levels
Clozapine-induced agranulocytosis
The most significant concern with clozapine is drug-induced agranulocytosis, a serious condition where the bone marrow doesn’t produce enough neutrophils and patients become vulnerable to severe infections. Clozapine-induced agranulocytosis (defined as ANC <500/µL) occurs in about 0.8% of patients (Mijovic A et al, Ann Hematol 2020;99(11):2477–2482). Symptoms include fever, sore throat, and mouth ulcers, though some patients remain asymptomatic. Mortality is estimated at about 3%.
The risk is highest in the first six months of treatment, so check your patient’s ANC every week for the first six months. At six months, you can reduce the ANC monitoring to every two weeks, and by a year of treatment, monthly monitoring suffices. However, if your patient misses over 30 days of clozapine and then resumes it, you’ll need to restart the monitoring schedule from the beginning (ie, weekly).
If your patient’s ANC drops, you will need to increase the frequency of monitoring, possibly needing to stop the clozapine altogether if the ANC drops too low (see “ANC Monitoring Guidelines” table). If your patient develops severe neutropenia/agranulocytosis, immediately stop the clozapine and transfer the patient to a medical ward with close hematological follow-up. Patients are typically treated with granulocyte colony-stimulating factor, even though this treatment is not FDA approved, since there is some evidence it may shorten the neutropenic phase. Clozapine-induced agranulocytosis lasts an average of 12 days.
If the benefits significantly outweigh the risks, you can prescribe clozapine to a patient who’s experienced agranulocytosis. Restart the monitoring schedule as if you were beginning treatment for a new patient.
Other side effects
Clozapine’s most common side effects are sedation, tachycardia, drooling, and constipation. Other side effects involve the central nervous system (dizziness, headaches, seizures) or are cardiovascular (hypotension, myocarditis), autonomic (sweating, dry mouth), or gastrointestinal (nausea) in nature. Also watch for elevation of liver enzymes since clozapine can cause hepatotoxicity.
Many side effects diminish over the first four to six weeks of treatment. Dividing the dose and prescribing higher doses at bedtime help to minimize side effects.
Drooling (sialorrhea)
You can try sublingual atropine, which is quick in onset and easy to administer (Van der Poorten T et al, Clin Case Rep 2019;7(11):2108–2113). Patients can use ophthalmic atropine 1% and administer one to three drops under their tongue three or four times daily. Other options include glycopyrrolate or supportive measures, such as sugar-free gum or a towel laid on the patient’s pillow.
Constipation
This is an often-underestimated risk of clozapine that can progress to intestinal obstruction and ischemic bowel disease. In fact, the FDA has released a warning about this potential side effect (www.tinyurl.com/4ybttdmf). I strongly recommend a prophylactic bowel regimen for patients, such as daily polyethylene glycol (Miralax), a stool softener, or senna, and avoiding bulk-forming agents like Metamucil.
Seizures
Risk is dose dependent, so titrate slowly and don’t prescribe doses that are higher than necessary. The annual incidence of seizures in patients taking clozapine is estimated at 5% (Correll et al, 2022). At higher doses or levels, consider seizure prophylaxis with valproic acid.
Metabolic syndrome and diabetes
Clozapine increases risk, so monitor blood sugars regularly and obtain your patients’ weight and vital signs (see “Clozapine Side Effects: Monitoring Recommendations”). Also, educate your patients about the importance of regular exercise and healthy eating.
Cardiovascular effects
The risk for myocarditis and cardiomyopathy is highest in the first month of clozapine treatment. Monitor troponins every week for the first month and ask about symptoms like chest pain and shortness of breath. Some recommendations include measuring C-reactive protein (CRP), since the combination of elevated CRP and elevated troponins (twice the upper limit of normal) is highly sensitive in detecting clozapine-induced myocarditis (Ronaldson KJ et al, Aust N Z J Psychiatry 2011;45(6):458–465). If troponins are elevated, stop clozapine and transfer the patient to a medical ward for further evaluation and treatment (which may include diuretics). Of all the second-generation agents, clozapine produces the highest risk of orthostatic hypotension, so be cautious when prescribing it to vulnerable populations like elderly patients. On the other hand, clozapine does not appear to cause clinically significant effects on the QT interval.
Special populations
Clozapine has an FDA Use in Pregnancy rating of B, based on animal studies, but we know very little about its safety in humans, so it’s best avoided in pregnant patients. It is present in breast milk, so breastfeeding is not recommended.
With older adults, monitor closely for orthostatic hypotension, tachycardia, and other anticholinergic side  effects like urinary retention. Older adult patients require lower doses, given their decreased kidney and liver function. Clozapine has a black box warning for increased risk of death when used for dementia-related psychosis.
effects like urinary retention. Older adult patients require lower doses, given their decreased kidney and liver function. Clozapine has a black box warning for increased risk of death when used for dementia-related psychosis.
Watch closely for hypotension in patients taking antihypertensives or who have a history of heart disease. Don’t prescribe clozapine for patients with a history of agranulocytosis, a history of hypersensitivity to clozapine, or a history of myocarditis or cardiomyopathy.
While clozapine does not seem to increase the risk of serious COVID-19 infection, patients with COVID-19 on clozapine have been found to have lower ANC and a potentially dangerous elevation in clozapine levels (Veerman SRT et al, Pharmacopsychiatry 2022;55(1):48–56). Monitor patients with COVID-19 closely for adverse events and decrease the clozapine dose by 50% until they have gone three days without a fever (Giles G et al, Schizophr Bull 2023;49(1):53–67).
CARLAT VERDICT
Clozapine is a highly effective drug for schizophrenia and suicidal behavior, but be sure to closely monitor neutrophil counts and watch for potentially serious side effects, including cardiomyopathy and seizures. Start with a low dosage, titrate slowly, and monitor patients regularly for weight gain, elevated blood sugars, and other signs of metabolic syndrome.



_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



