Psychiatric Consultation to Children and Adolescents on Pediatric Units: A Primer
Pediatric consultation-liaison (C-L) psychiatry is a unique subspecialty, bridging the fields of psychiatry, pediatrics, and child development. In this review, we share tips for the management of pediatric C-L psychiatry consults in inpatient pediatric settings.
The consultation process
When children are sick, it can be tough for them to share their medical history or follow treatment recommendations. It’s crucial to involve the child’s family, caregivers, and treatment team, and it’s equally important to include the child to get a complete understanding of their condition and encourage autonomy. The following are our recommendations for how to approach the consultation process.
Get consent
Make sure to have consent from minors’ legal guardians before conducting evaluations or recommending treatment. If you’re unsure about who has decision-making authority, the hospital social work team can verify that information.
Explain the situation
Tell the child and family who you are and why you are there. Children may not understand the medical system and are likely to be confused about why you are suddenly in the room asking them questions. We often say that we are “talking doctors” and help to support children who are hospitalized, given the stresses of being in the hospital.
Decide who should be present
Ask the child if they prefer to have their parent or caregiver present to start the interview or to speak alone. It’s important to speak with the child separately at some point during the evaluation to ask about safety, trauma, substance use, and sexual history if indicated, and to get the parent’s or caregiver’s perspective separately as well.
Below, we will review some of the most common reasons for pediatric psychiatric consultation.
Suicide risk assessment
Suicide is a sensitive topic and can be uncomfortable for parents and children to discuss.
Tips to guide the conversation
- Combine empathic listening with frank questioning guided by screening tools like the Columbia Suicide Severity Rating Scale (see “Suicide in Children and Adolescents” article in this issue for links to this and other screening tools).
- Use age-appropriate language when asking kids about suicidality. For example: “Sometimes when people feel really sad, they might have thoughts of wanting to hurt themselves or not wanting to live anymore. Have you ever felt this way?”
- Ask about prior self-harm, including non-suicidal self-injury, since a child who has attempted suicide before is at higher risk of a future attempt. For an adolescent, you might say “Sometimes people tell me they harm themselves for reasons other than trying to end their life. Have you ever done this?”
- Ask about home access to firearms, substances, sharp objects, and medications, including over-the-counter medications.
- Certain psychiatric issues increase the risk of suicide in children. You should screen for mood disorders (either unipolar or bipolar depression), ADHD, and a history of impulsivity or trauma.
Safety interventions
If you conclude that your patient is at high risk for suicide or self-harm, consider the following interventions:
- Suggest bringing in a staff member to provide constant observation
- Mitigate potentially hazardous items (eg, ask that lines or cords be removed from the hospital room)
- Adjust psychiatric medications to target symptoms such as anxiety and irritability
- Recommend the patient be admitted to a psychiatric unit once medically stabilized, and placed on an involuntary hold if necessary for the child’s safety
Chronic medical illnesses
You may be asked to see children with chronic medical illnesses (eg, cystic fibrosis, type 1 diabetes, or sickle cell anemia) as they often suffer with anxiety or depression. You can help a child and family cope with illness by providing a listening ear, using bedside psychotherapy and medication interventions, and liaising with the other medical teams. Involve the hospital’s child life specialists, as they help children and families adjust to illness, hospital stays, and procedures.
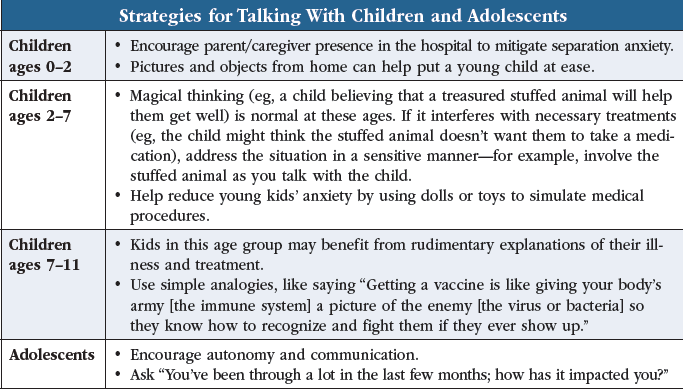
Tailor your recommendations based on the child’s developmental stage (see table).
Medically unexplained symptoms
Pediatrics teams may consult you when a child presents with medically unexplained symptoms.
Somatic symptom and related disorders (SSRDs)
Somatization is normal—lots of kids complain of occasional stomachaches or dizziness. But its interference with daily functioning (eg, a child frequently missing school because of these symptoms) could indicate an SSRD, like illness anxiety disorder, functional neurologic disorder, or factitious disorder. Illness anxiety disorder is characterized by an extreme preoccupation with physical symptoms, like pain or fatigue, leading to emotional distress and poor functioning. The child may or may not have an associated medical condition, but their reaction to the symptoms is excessive. SSRDs often present in children with other diagnosed medical conditions, so we are careful to ensure that the patient undergoes thorough multidisciplinary assessments.
What should you ask a child who may have an SSRD? Explore possible stressors and psychosocial contributions to the child’s illness, but remember that due to the complex nature of the mind-body connection, a clear trigger frequently is not found. Has the child recently moved to a new school? Have there been recent changes in the household, such as the arrival of a baby brother or sister? By addressing stressors and talking to the child and parent about how emotional distress can manifest as body symptoms, you can help resolve the symptoms of SSRDs. Multidisciplinary support for SSRDs includes regular appointments with medical providers, skills-based psychotherapy (like cognitive behavioral therapy), and physical therapy and other rehabilitative services.
Factitious disorder imposed on another
Factitious disorder imposed on another (formerly called Munchausen by proxy), though rare, is a form of medical child abuse that may be the cause of medically unexplained symptoms. If you suspect abuse, help assemble a multidisciplinary team for evaluation, including child protection and legal teams.
Autism and other developmental conditions
For autistic children and children with other developmental or behavioral conditions, work with the parents/guardian and treatment team to identify and minimize potential triggers for behavioral issues. Triggers include sensory overload (crowded, noisy, or brightly lit environments) and changes in routine. It’s also helpful to identify comfort items or media, like a favorite blanket or song. If needed, you can recommend medication options to prevent or mitigate behavioral dysregulation.
Children and adolescents with substance use disorders
Rates of pediatric substance use have risen in recent years, as has the rate of children presenting to medical hospitals for related complications. C-L evaluation of pediatric substance use presents a unique opportunity for intervention. Children who use substances have higher rates of medical complications, but less frequent access to longitudinal outpatient care than adults. You can help these patients by:
- Screening for substance use using a systematic and comprehensive tool, eg, the Screening to Brief Intervention (S2BI) (www.nida.nih.gov/s2bi/)
- Engaging candidly with patients and families and providing psychoeducation on the risk of ongoing substance use
- Using psychopharmacologic interventions to treat substance use disorder and comorbid psychiatric conditions
- Connecting children and families with longitudinal substance use treatment
When talking with patients and families, use reflective listening and motivational interviewing. Be careful to avoid blame and present the issue as a challenge the family must address together.
Eating disorders
You’ll be part of the medical team that helps diagnose and establish treatment plans for patients with eating disorders. Besides anorexia nervosa and bulimia nervosa, you can help identify avoidant/restrictive food intake disorder (ARFID), which is marked by restrictive eating without impairment of body image. The prevalence of ARFID is estimated at about 3%, but rates are much higher among children with neurodevelopmental disorders (Kurz S et al, Eur Child Adolesc Psychiatry 2015;24(7):779–785).
Children admitted to pediatric units with an eating disorder are often on a refeeding protocol. They require close monitoring for refeeding syndrome—a potentially life-threatening condition whereby metabolic abnormalities occur if food is introduced too quickly after a period of starvation. Once patients are medically stabilized, coordinate transfer to a psychiatric inpatient or residential eating disorder facility.
Altered mental status (AMS)
AMS is another condition you might encounter on pediatric floors. While there are many potential causes, we will focus on delirium, catatonia, and autoimmune encephalitis.
Delirium
Pediatric delirium occurs in at least 20%–25% of critically ill patients. It is associated with worse outcomes, including higher rates of mortality, and is more likely seen among children with neurodevelopmental disorders (Traube C et al, Crit Care Med 2014;42(3):656–663; Becker JE et al, Psychosomatics 2020;61(5):467–480). Like in adults, symptoms include fluctuating changes in mental status, inattention, altered level of consciousness, and disorganized thinking. To screen for delirium in children:
- Ask basic orientation questions for person, place, and time
- Give simple instructions, like saying “Squeeze my hand only when I say ‘A’” and proceeding to list several letters in a row
- Assess thought organization with questions like “Is ice cream hot?” “Do birds fly?” (for more information, go to: www.tinyurl.com/3mefpttr)
Start with non-psychopharmacologic interventions and be sure to:
- Identify and treat underlying potential causes of delirium (eg, infection, seizure, substance use)
- Remove or limit medications that can worsen delirium and confusion (eg, opioids, anticholinergics, benzodiazepines)
- Make environmental modifications: Provide good lighting, signs, and clocks for children who can tell time; ensure window shades are up during daytime hours; etc
- Reorient frequently: Give children reminders of where they are and of staff names and roles
- Address communication/sensory difficulties (eg, provide a communication board for children unable to speak, involve speech or occupational therapy, etc)
Pharmacologic treatments include antipsychotics for hyperactive delirium (eg, quetiapine, risperidone) or alpha-2 agonists (eg, clonidine, guanfacine). Consider melatonin to address sleep disturbance (Becker et al, 2020).
Catatonia
Like delirium, catatonia is also associated with worse medical and psychiatric outcomes in children. Evaluate for catatonia in children like you would adults—using the Bush-Francis scale. Look for:
- Immobility
- Mutism
- Fixed gaze
- Erratic, non-purposeful movements
- Odd mannerisms or facial expressions
- Mimicry of others’ speech or gestures
When treating catatonia in children and adolescents:
- Evaluate for and treat potential underlying medical or neurologic conditions; in children with autism or other developmental disorders, explore whether atypical movements or postures are part of a child’s baseline
- Discontinue or reduce the use of antipsychotics
- Administer a lorazepam challenge of 2 mg IV; if positive, increase the frequency and doses of lorazepam until symptom remission is achieved, monitoring carefully for sedation with escalating doses
- Consider electroconvulsive therapy (ECT) if the above interventions are ineffective; note that laws around administration of ECT to minors vary by state and may preclude its use
Autoimmune encephalitis
Autoimmune encephalitis is a condition in which the immune system mistakenly attacks the brain, causing symptoms like confusion, memory loss, seizures, and even psychosis.
Work closely with pediatrics and neurology to complete the workup, which includes brain imaging, electroencephalogram, and serum and cerebrospinal fluid autoantibody screens. Remember the following:
- Immunotherapy, including corticosteroids, plasma exchange, and IV immunoglobulins, is the main treatment
- Provide symptom-focused therapies targeting anxiety and agitation
- Avoid antipsychotics because these patients have a higher risk of developing neuroleptic malignant syndrome
- Be cautious when using benzodiazepines as they can worsen delirium
CARLAT VERDICT
Principal reasons for pediatric C-L consultation include suicide risk assessments,chronic medical illnesses, medically unexplained symptoms, AMS,eating disorders, and substance use dis- orders. Involve the child’s caregivers in your evaluations while also promoting autonomy for older children. Be sure to obtain consent before any evaluations or procedures involving minors, and assist medical teams in identifying and avoid- ing triggers (such as noisy or crowded environments) for children with develop mental disorders


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



