Home » A Look at the Latest Antidepressant Meta-Analysis
A Look at the Latest Antidepressant Meta-Analysis
June 1, 2018
From The Carlat Psychiatry Report
Adam Strassberg, MD
Psychiatrist in private practice in Palo Alto, CA. Contributing writer to the Carlat newsletters.
Dr. Strassberg has disclosed that he has no relevant financial or other interests in any commercial companies pertaining to this educational activity.
You may have read about the meta-analysis published in Lancet earlier this year on the efficacy evidence for all antidepressants (Cipriani A et al, Lancet 2018;391(10128):1357–1366). It’s a complicated paper, and in this article, we’ll take a closer look at it and give you our take on the bottom line.
The authors did a systematic review and meta-analysis, searching published and unpublished, double-blind, randomized controlled trials up to January 2016, notably also including the largest amount of unpublished data to date. Both placebo-controlled and head-to-head trials were included across 21 antidepressants, and each evaluated monotherapy for the acute treatment of adults with unipolar major depression. In total, the authors analyzed 522 trials covering 116,477 participants.
The primary outcomes were “efficacy” and “acceptability.” Efficacy was defined as the response rate at 8 weeks as measured by a reduction of ≥ 50% of the total score on a standardized depression rating scale. Acceptability was defined as treatment discontinuation as measured by the proportion of patients who withdrew from a study for any reason by 8 weeks.
Here are some of the more interesting findings:
How might this study change the way you choose antidepressants? To better understand the analysis, TCPR interviewed John Ioannidis, MD, one of the study’s authors, and Professor of Medicine, Health Research and Policy, and Biomedical Data Science at the Stanford University School of Medicine. Dr. Ioannidis offered the following insight:
TCPR Verdict: No big surprises in this study, which shows that SSRIs have the best combination of efficacy and tolerability—though efficacy is modest.
General PsychiatryThe authors did a systematic review and meta-analysis, searching published and unpublished, double-blind, randomized controlled trials up to January 2016, notably also including the largest amount of unpublished data to date. Both placebo-controlled and head-to-head trials were included across 21 antidepressants, and each evaluated monotherapy for the acute treatment of adults with unipolar major depression. In total, the authors analyzed 522 trials covering 116,477 participants.
The primary outcomes were “efficacy” and “acceptability.” Efficacy was defined as the response rate at 8 weeks as measured by a reduction of ≥ 50% of the total score on a standardized depression rating scale. Acceptability was defined as treatment discontinuation as measured by the proportion of patients who withdrew from a study for any reason by 8 weeks.
Here are some of the more interesting findings:
- All antidepressants were more effective than placebo, with odds ratios (OR) ranging from 2.13 for amitriptyline to 1.37 for reboxetine (a norepinephrine reuptake inhibitor not approved in the US). For acceptability, only agomelatine (an atypical agent not approved in the US, OR 0.84) and fluoxetine (OR 0.88) were associated with fewer dropouts than placebo, while clomipramine was associated with more dropouts than placebo (OR 1.30).
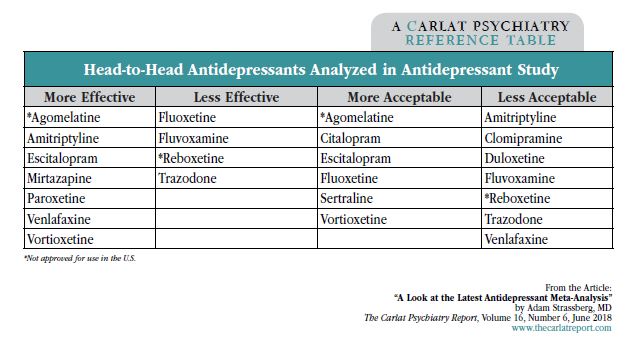
- In head-to-head trials, certain antidepressants were more efficacious than others, and several had more acceptability in terms of dropout rates due to side effects. Agomelatine, amitriptyline, escitalopram, mirtazapine, paroxetine, venlafaxine, and vortioxetine were more effective than other antidepressants (ORs 1.19–1.96), while fluoxetine, fluvoxamine, reboxetine, and trazodone were least efficacious (ORs 0.51–0.84). For tolerability, agomelatine, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine were more acceptable than other agents (ORs 0.43–0.77), while dropout rates were highest for amitriptyline, clomipramine, duloxetine, fluvoxamine, reboxetine, trazodone, and venlafaxine (ORs 1.30–2.32).
- The authors don’t directly recommend any drugs over others—they mostly present significant amounts of data. However, in their discussion, they note “some antidepressants, such as escitalopram, mirtazapine, paroxetine, agomelatine, and sertraline had a relatively higher response and lower dropout rates than other antidepressants. By contrast, reboxetine, trazodone, and fluvoxamine were associated with generally inferior efficacy and acceptability profiles compared with other antidepressants.”
- Industry funding was not associated with substantial differences in outcomes for either response or dropout rates.
How might this study change the way you choose antidepressants? To better understand the analysis, TCPR interviewed John Ioannidis, MD, one of the study’s authors, and Professor of Medicine, Health Research and Policy, and Biomedical Data Science at the Stanford University School of Medicine. Dr. Ioannidis offered the following insight:
- The results overall suggest that antidepressants on average have modest/small efficacy.
- Looking at individual antidepressants, mirtazapine ranks close to the top for efficacy and is about average for acceptability; amitriptyline ranks at the top in efficacy and is ranked a bit better than average for acceptability; venlafaxine ranks high on efficacy but low on acceptability; and paroxetine ranks modestly, roughly average in both. You can use these rankings to inform your decisions about which antidepressants to choose.
- The differences between antidepressants were very modest, even smaller than the differences between antidepressants and placebo. These differences may represent chance or bias.
- The meta-analysis does not support the idea that antidepressants are entirely useless. On average, they do have small/modest benefit. At the same time, the meta-analysis focused on short-term treatment of patients with well-documented major depression, typically moderate or severe major depression. Also, this meta-analysis provides no evidence—positive or negative—regarding the long-term use of antidepressants.
TCPR Verdict: No big surprises in this study, which shows that SSRIs have the best combination of efficacy and tolerability—though efficacy is modest.
Issue Date: June 1, 2018
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



