Home » The “Whole-Patient” Approach to Psychiatric Diagnosis
The “Whole-Patient” Approach to Psychiatric Diagnosis
May 1, 2014
From The Carlat Psychiatry Report
Margaret S. Chisolm, MD
Associate Professor, Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore, MD
Dr. Chisholm has disclosed that she receives book royalties from the JHU Press. Dr. Balt has reviewed this article and found no evidence of bias in this educational activity.
This month marks the one-year anniversary of the publication of DSM-5. Designed as an atheoretical research tool to establish a reliable and consistent way to make psychiatric diagnoses without any comment as to their underlying cause, the DSM has become the go-to clinical diagnostic resource for mental health professionals.
Unfortunately, many are unaware of the volume’s scientific limitations, particularly its lack of validity. Fourteen years in the making, this latest version (DSM-5) has been the subject of intense global scrutiny and criticism both before and since publication (see, for instance, the Expert Q&A with Allen Frances in this issue).
Some are concerned that the DSM-5 will make more people mentally ill; others, that the formerly ill will be “cured,” jeopardizing their access to continuing care. Unfortunately, not only has this attention cast a light on the inadequacies of the DSM, but it has also further undermined the credibility of our field, to the detriment of our patients.
An Alternative To DSM?
Alongside DSM, another conceptual model has risen, one based on concepts originally developed by Adolf Meyer and Karl Jaspers in the early 20th century. In the 1980s, these ideas were organized and later were described in the book, The Perspectives of Psychiatry, published in 1998 (Johns Hopkins University Press). The Perspectives of Psychiatry’s authors, Paul McHugh and Phillip Slavney, have steadfastly viewed the DSM system as fundamentally flawed and have consistently expressed concern about its negative impact on the field.
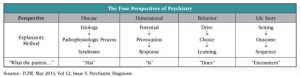
Wishing to move US psychiatry beyond the DSM, they have voiced the utility of their more comprehensive framework for understanding psychiatric conditions (see, for instance, McHugh PR and Slavney PR, New Engl J Med 2012;366:1853–1855, available at bit.ly/1lZlf2Q). Their model translates into a pragmatic “whole-patient” approach to psychiatric diagnosis in which a clinician considers every psychiatric patient from four points of view (disease, dimensional, behavior, and life story) to understand how that patient’s thoughts, feelings, and behavior may have gone awry.
The Whole-Patient Approach
The whole-patient approach (sometimes called the “Perspectives of Psychiatry” approach) acknowledges that, whereas general medical conditions are consistently understood as diseases arising from a diseased entity or “broken part,” not all psychiatric conditions can be understood that way. Different psychiatric disorders have different natures.
This systematic whole-patient approach differs from eclectic holistic approaches, such as George Engel’s biopsychosocial model (Engel GL, Am J Psychiatry 1980;137:535), which merely provides a list of “ingredients” relevant to psychiatric diagnosis. Instead, the whole-patient approach also provides the recipe—a sequential, comprehensive series of steps—to turn that list of ingredients into personalized formulations for individual patients.
The following are the four perspectives to consider for each psychiatric patient when using the whole-patient approach to diagnosis.
Disease perspective. Physicians are most familiar with the disease perspective portion of this model. From this point of view, the etiology of a patient’s troubles is understood as arising from a pathophysiologic process within a specific organ or organ system, which leads to the presenting syndrome.
For example, the disruption in mental life faced by patients with dementia may be understood as developing from physical changes in the brain. The questions one asks when approaching a patient from the disease perspective are “What is the broken part? and, “What disease does the patient have?”
Dimensional perspective. For many psychiatric conditions, the disease perspective is inadequate to fully explain the distress with which patients present. The dimensional perspective thus provides a framework for understanding those psychiatric conditions that arise from variations in an individual’s physical or psychological attributes. These endowments may lead the patient to react to certain things with an individual set of pathological responses.
Someone who has either too little or an overabundance of a particular personality trait may be especially vulnerable to experiencing psychiatric distress. Such a patient’s symptoms are not from a “broken part” in the brain, and a psychiatrist can best serve this type of patient by asking, “Given my patient’s particular strengths and vulnerabilities, how can I best guide him toward success?” He must attempt to understand what kind of person the patient is.
Behavior perspective. As its name implies, the behavior perspective can be helpful in understanding psychiatric problems that stem from a maladaptive behavior. This perspective is based on the concept that an individual’s psychological drives, shaped partly by conditioned learning, influence his or her choice in whether or not to engage in goal-directed behavior.
Recognizing maladaptive behavior in patients, and considering the factors that can initiate and sustain such behaviors, is critical to treating many psychiatric disorders, including substance use and eating disorders. The behavior perspective prompts psychiatrists to ask, “How can my patient’s distress be explained by, and how can I help by changing, what he does?”
Life story perspective. Lastly, some individuals seeking psychiatric help are burdened not by a disease they have, by who they are, or by things they do, but by what they have encountered in life. Such psychiatric disorders are best understood by using the life story perspective. This perspective uses the logic of narrative—a sequence of events within a particular setting and leading to a specific outcome—to understand a patient’s psychiatric state.
For example, a recent widow may seek treatment for feelings of sadness following the death of her husband. Using the life-story perspective, her psychiatrist may understand the presenting symptoms as arising from the loss and use psychotherapy to help the patient “rescript” her life story in a way that enables her to regain a feeling of mastery over her circumstances. In the life story perspective, the psychiatrist must consider what the patient encounters.
A Case Study of the Whole-Patient Approach
To illustrate how a common patient presentation might be addressed using this approach to psychiatric diagnosis, consider the case of a 60-year-old female social worker who comes for outpatient evaluation for worsening irritability and depressed mood. Of note, the patient was raised by a foster family until the age of 12 when, after a teacher suspected physical abuse, social services intervened and the patient was moved to her eventual adoptive family. They provided a loving and secure home, although they passed away not long after the patient graduated from high school, leaving her without resources for college.
According to the patient’s daughter, her mother had always been able to weather life’s difficulties. She created a loving and stable family of her own and enjoyed a close network of friends. She never used any illicit substance and did not drink alcohol.
In fact, the patient’s life was stable and relatively uneventful until five months ago when her husband of 35 years was diagnosed with dementia, after worsening confusion over the past year. Since her husband’s diagnosis, the patient’s mood has been more irritable and sad. She has had more difficulty falling asleep, and has lost weight.
On mental status examination, her mood is sad and does not brighten as the interview progresses. She cries frequently, especially when discussing her husband’s condition. She describes poor energy/motivation and difficulty concentrating. She feels guilty and has little hope for the future. She denies thoughts of suicide and evidences no psychotic symptoms.
In this case, you must consider the patient from the life story perspective as a way of understanding her symptoms. The patient has endured a number of childhood stressors, both psychological and physical, but she had the resilience and optimism to overcome these past adversities.
Her current symptoms follow on the heels of her husband’s diagnosis with dementia. It may be tempting to propose that her symptoms may be the result of this event, but they do not fit with how she has reacted to stresses in the past. As a result, it would be prudent to defer any conclusion about the cause of her present condition until considering her problem from the other perspectives.
Because she does not appear to be on any extreme of either cognition or temperament (confirmed by her daughter) and has successfully weathered other challenges in the past, it does not appear that the patient’s present condition is arising from who she is as a person, and thus cannot be understood primarily from the dimensional perspective.
The behavior perspective also says little about her current presentation. She has no evidence of primary sleep, eating, or sexual disorders; and denies the use of licit and illicit substances.
This brings you to the disease perspective. Disease reasoning begins with the identification of a clinical syndrome, so the first thing one needs to decide is whether the patient’s current psychiatric presentation fits well with a clinical syndrome. The decline in her mood, sleep, appetite, energy, concentration, along with guilt and hopelessness, may indeed represent a case of major depressive disorder.
The fact that a stressful circumstance preceded her symptoms in no way changes the fact that they add up to a clinical syndrome. Given that this patient’s syndrome emerged in the context of her husband’s diagnosis, you can construct a plausible, meaningful narrative to explain her syndrome as arising from this stressful life circumstance.
However, you must consider whether or not the symptoms represent a new theme in her life. If so, her symptoms may be better explained as arising from an abnormality in the structure or function of her brain rather than from the stressful life event that she has encountered. Depressive symptoms often arise in the setting of stressful life events and, although patients and clinicians often draw on storytelling to help understand these symptoms, not every story we tell may be true.
Clinicians risk falling into a “trap of meaning” (Lyketsos & Chisolm, JAMA 2009;302:432–433) when they invoke meaningful explanations to understand new symptoms that can also be caused by a disease process. In this case, a clinician shouldn’t let a meaningful explanation obscure recognition that the true nature and origin of a patient’s suffering can be the clinical syndrome of major depressive disorder.
Although the patient’s depressive symptoms may be partly due to her husband’s recent diagnosis of dementia, which may have overpowered the resilience she had demonstrated through most of her life, they are most likely not solely due to this. Rather, the symptoms probably arise from the interaction of an unknown pathologic process in her brain provoked by stressful occurrences, for which a combination of psychotherapy and pharmacotherapy are indicated.
In Summary
The whole-patient approach incorporates all four perspectives—disease, dimensional, behavior, and life story—in a systematic and personal way. It enables you to understand your patient to a depth and breadth that is impossible to achieve with the DSM alone. Although the DSM organizes psychiatric conditions reliably, it is not enough to simply run through a check list of non-specific DSM signs and symptoms to make a diagnosis. Psychiatric illness doesn’t occur in a vacuum—it arises from and is shaped by an individual’s life.
TCPR’s Verdict: The whole-patient approach helps to sharpen and clarify clinical reasoning about patients, especially those with chaotic lives and multiple problems. It enables treatment recommendations tailored to the specific person and has been disseminated widely to help psychiatrists think more deeply about their patients. When used in tandem with the DSM, it allows for individualized care and productive collaboration with the patient.
General PsychiatryUnfortunately, many are unaware of the volume’s scientific limitations, particularly its lack of validity. Fourteen years in the making, this latest version (DSM-5) has been the subject of intense global scrutiny and criticism both before and since publication (see, for instance, the Expert Q&A with Allen Frances in this issue).
Some are concerned that the DSM-5 will make more people mentally ill; others, that the formerly ill will be “cured,” jeopardizing their access to continuing care. Unfortunately, not only has this attention cast a light on the inadequacies of the DSM, but it has also further undermined the credibility of our field, to the detriment of our patients.
An Alternative To DSM?
Alongside DSM, another conceptual model has risen, one based on concepts originally developed by Adolf Meyer and Karl Jaspers in the early 20th century. In the 1980s, these ideas were organized and later were described in the book, The Perspectives of Psychiatry, published in 1998 (Johns Hopkins University Press). The Perspectives of Psychiatry’s authors, Paul McHugh and Phillip Slavney, have steadfastly viewed the DSM system as fundamentally flawed and have consistently expressed concern about its negative impact on the field.
Wishing to move US psychiatry beyond the DSM, they have voiced the utility of their more comprehensive framework for understanding psychiatric conditions (see, for instance, McHugh PR and Slavney PR, New Engl J Med 2012;366:1853–1855, available at bit.ly/1lZlf2Q). Their model translates into a pragmatic “whole-patient” approach to psychiatric diagnosis in which a clinician considers every psychiatric patient from four points of view (disease, dimensional, behavior, and life story) to understand how that patient’s thoughts, feelings, and behavior may have gone awry.
The Whole-Patient Approach
The whole-patient approach (sometimes called the “Perspectives of Psychiatry” approach) acknowledges that, whereas general medical conditions are consistently understood as diseases arising from a diseased entity or “broken part,” not all psychiatric conditions can be understood that way. Different psychiatric disorders have different natures.
This systematic whole-patient approach differs from eclectic holistic approaches, such as George Engel’s biopsychosocial model (Engel GL, Am J Psychiatry 1980;137:535), which merely provides a list of “ingredients” relevant to psychiatric diagnosis. Instead, the whole-patient approach also provides the recipe—a sequential, comprehensive series of steps—to turn that list of ingredients into personalized formulations for individual patients.
The following are the four perspectives to consider for each psychiatric patient when using the whole-patient approach to diagnosis.
Disease perspective. Physicians are most familiar with the disease perspective portion of this model. From this point of view, the etiology of a patient’s troubles is understood as arising from a pathophysiologic process within a specific organ or organ system, which leads to the presenting syndrome.
For example, the disruption in mental life faced by patients with dementia may be understood as developing from physical changes in the brain. The questions one asks when approaching a patient from the disease perspective are “What is the broken part? and, “What disease does the patient have?”
Dimensional perspective. For many psychiatric conditions, the disease perspective is inadequate to fully explain the distress with which patients present. The dimensional perspective thus provides a framework for understanding those psychiatric conditions that arise from variations in an individual’s physical or psychological attributes. These endowments may lead the patient to react to certain things with an individual set of pathological responses.
Someone who has either too little or an overabundance of a particular personality trait may be especially vulnerable to experiencing psychiatric distress. Such a patient’s symptoms are not from a “broken part” in the brain, and a psychiatrist can best serve this type of patient by asking, “Given my patient’s particular strengths and vulnerabilities, how can I best guide him toward success?” He must attempt to understand what kind of person the patient is.
Behavior perspective. As its name implies, the behavior perspective can be helpful in understanding psychiatric problems that stem from a maladaptive behavior. This perspective is based on the concept that an individual’s psychological drives, shaped partly by conditioned learning, influence his or her choice in whether or not to engage in goal-directed behavior.
Recognizing maladaptive behavior in patients, and considering the factors that can initiate and sustain such behaviors, is critical to treating many psychiatric disorders, including substance use and eating disorders. The behavior perspective prompts psychiatrists to ask, “How can my patient’s distress be explained by, and how can I help by changing, what he does?”
Life story perspective. Lastly, some individuals seeking psychiatric help are burdened not by a disease they have, by who they are, or by things they do, but by what they have encountered in life. Such psychiatric disorders are best understood by using the life story perspective. This perspective uses the logic of narrative—a sequence of events within a particular setting and leading to a specific outcome—to understand a patient’s psychiatric state.
For example, a recent widow may seek treatment for feelings of sadness following the death of her husband. Using the life-story perspective, her psychiatrist may understand the presenting symptoms as arising from the loss and use psychotherapy to help the patient “rescript” her life story in a way that enables her to regain a feeling of mastery over her circumstances. In the life story perspective, the psychiatrist must consider what the patient encounters.
A Case Study of the Whole-Patient Approach
To illustrate how a common patient presentation might be addressed using this approach to psychiatric diagnosis, consider the case of a 60-year-old female social worker who comes for outpatient evaluation for worsening irritability and depressed mood. Of note, the patient was raised by a foster family until the age of 12 when, after a teacher suspected physical abuse, social services intervened and the patient was moved to her eventual adoptive family. They provided a loving and secure home, although they passed away not long after the patient graduated from high school, leaving her without resources for college.
According to the patient’s daughter, her mother had always been able to weather life’s difficulties. She created a loving and stable family of her own and enjoyed a close network of friends. She never used any illicit substance and did not drink alcohol.
In fact, the patient’s life was stable and relatively uneventful until five months ago when her husband of 35 years was diagnosed with dementia, after worsening confusion over the past year. Since her husband’s diagnosis, the patient’s mood has been more irritable and sad. She has had more difficulty falling asleep, and has lost weight.
On mental status examination, her mood is sad and does not brighten as the interview progresses. She cries frequently, especially when discussing her husband’s condition. She describes poor energy/motivation and difficulty concentrating. She feels guilty and has little hope for the future. She denies thoughts of suicide and evidences no psychotic symptoms.
In this case, you must consider the patient from the life story perspective as a way of understanding her symptoms. The patient has endured a number of childhood stressors, both psychological and physical, but she had the resilience and optimism to overcome these past adversities.
Her current symptoms follow on the heels of her husband’s diagnosis with dementia. It may be tempting to propose that her symptoms may be the result of this event, but they do not fit with how she has reacted to stresses in the past. As a result, it would be prudent to defer any conclusion about the cause of her present condition until considering her problem from the other perspectives.
Because she does not appear to be on any extreme of either cognition or temperament (confirmed by her daughter) and has successfully weathered other challenges in the past, it does not appear that the patient’s present condition is arising from who she is as a person, and thus cannot be understood primarily from the dimensional perspective.
The behavior perspective also says little about her current presentation. She has no evidence of primary sleep, eating, or sexual disorders; and denies the use of licit and illicit substances.
This brings you to the disease perspective. Disease reasoning begins with the identification of a clinical syndrome, so the first thing one needs to decide is whether the patient’s current psychiatric presentation fits well with a clinical syndrome. The decline in her mood, sleep, appetite, energy, concentration, along with guilt and hopelessness, may indeed represent a case of major depressive disorder.
The fact that a stressful circumstance preceded her symptoms in no way changes the fact that they add up to a clinical syndrome. Given that this patient’s syndrome emerged in the context of her husband’s diagnosis, you can construct a plausible, meaningful narrative to explain her syndrome as arising from this stressful life circumstance.
However, you must consider whether or not the symptoms represent a new theme in her life. If so, her symptoms may be better explained as arising from an abnormality in the structure or function of her brain rather than from the stressful life event that she has encountered. Depressive symptoms often arise in the setting of stressful life events and, although patients and clinicians often draw on storytelling to help understand these symptoms, not every story we tell may be true.
Clinicians risk falling into a “trap of meaning” (Lyketsos & Chisolm, JAMA 2009;302:432–433) when they invoke meaningful explanations to understand new symptoms that can also be caused by a disease process. In this case, a clinician shouldn’t let a meaningful explanation obscure recognition that the true nature and origin of a patient’s suffering can be the clinical syndrome of major depressive disorder.
Although the patient’s depressive symptoms may be partly due to her husband’s recent diagnosis of dementia, which may have overpowered the resilience she had demonstrated through most of her life, they are most likely not solely due to this. Rather, the symptoms probably arise from the interaction of an unknown pathologic process in her brain provoked by stressful occurrences, for which a combination of psychotherapy and pharmacotherapy are indicated.
In Summary
The whole-patient approach incorporates all four perspectives—disease, dimensional, behavior, and life story—in a systematic and personal way. It enables you to understand your patient to a depth and breadth that is impossible to achieve with the DSM alone. Although the DSM organizes psychiatric conditions reliably, it is not enough to simply run through a check list of non-specific DSM signs and symptoms to make a diagnosis. Psychiatric illness doesn’t occur in a vacuum—it arises from and is shaped by an individual’s life.
TCPR’s Verdict: The whole-patient approach helps to sharpen and clarify clinical reasoning about patients, especially those with chaotic lives and multiple problems. It enables treatment recommendations tailored to the specific person and has been disseminated widely to help psychiatrists think more deeply about their patients. When used in tandem with the DSM, it allows for individualized care and productive collaboration with the patient.
KEYWORDS dsm practice-tools-and-tips
Issue Date: May 1, 2014
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)



